-
Property & Casualty
Property & Casualty Overview

Property & Casualty
We offer a full range of reinsurance products and the expertise of our talented reinsurance team.
Expertise
Publication
Florida Property Tort Reforms – Evolving Conditions
Publication
Is Human Trafficking the Next Big Liability Exposure for Insurers?
Publication
When Likes Turn to Lawsuits – Social Media Addiction and the Insurance Fallout
Publication
Generative Artificial Intelligence and Its Implications for Weather and Climate Risk Management in Insurance
Publication
Engineered Stone – A Real Emergence of Silicosis
Publication
Who’s Really Behind That Lawsuit? – Claims Handling Challenges From Third-Party Litigation Funding -
Life & Health
Life & Health Overview

Life & Health
We offer a full range of reinsurance products and the expertise of our talented reinsurance team.

Publication
Understanding Physician Contracts When Underwriting Disability Insurance
Publication
Voice Analytics – Insurance Industry Applications [Webinar]
Publication
GLP-1 Receptor Agonists – From Evolution to Revolution U.S. Industry Events
U.S. Industry Events
Publication
Always On: Understanding New Age Addictions and Their Implications for Disability Insurance
Publication
Dying Gracefully – Legal, Ethical, and Insurance Perspectives on Medical Assistance in Dying -
Knowledge Center
Knowledge Center Overview

Knowledge Center
Our global experts share their insights on insurance industry topics.
Trending Topics -
About Us
About Us OverviewCorporate Information

Meet Gen Re
Gen Re delivers reinsurance solutions to the Life & Health and Property & Casualty insurance industries.
- Careers Careers
Mortality and Morbidity at the End of Life’s Road

June 20, 2019
Jean-Marc Fix
English
How long will I live? It’s a question that humans have pondered since the dawn of time. From palmistry to the latest health fads, we have found more or less satisfactory answers. Those of us in the Life industry, as students of mortality, are interested in a similar question: How does mortality vary and evolve by age and with time?
For a long time, actuaries have identified lower mortality with the younger and middle ages; it is only in the last three or four decades that we have appreciated the impact of mortality reduction at older ages. As we try to understand this impact, a vexing question comes to mind: Do humans have an expiry date? Implicitly, our life tables ended for many years by the ominous qω=1, everyone dies at age omega.
We have pushed ω further and further with each successive actuarial mortality table and now have disposed of it altogether, in favor of a constant, which empirically seems to be close to 0.5. Yet the question remains: Is there a maximum or will the record of 122 years held by Jeanne Calment, a French supercentenarian, stand unbeatable as it has for more than 20 years?
One way to observe what happens to the mortality for a given birth year is to look at the percentage of survivors by year until there are none. This is called the survival curve. For many years and in all developed countries, the curve has become more rectangular.
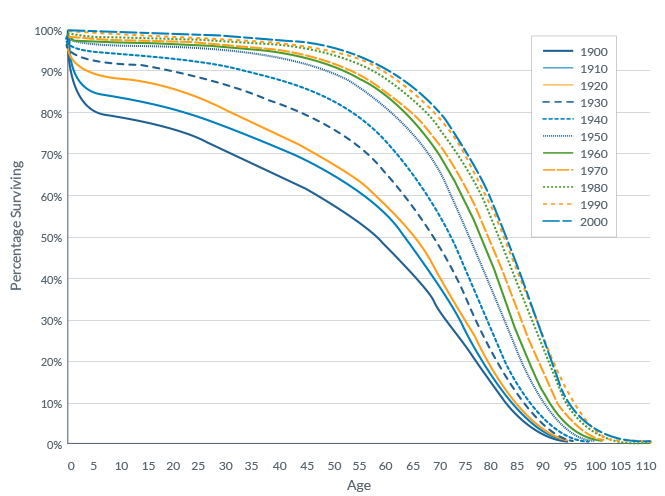
This implies that people survive to an advanced age and die rapidly thereafter. This is generally associated with what is called the compression of mortality, where deaths are concentrated around the modal age of death, the age that has the most death.
For low mortality countries (i.e., highly-developed nations), there has been some evidence of compression for several decades, depending on how you mathematically define it. The modal age of death, and the number of deaths concentrated around that age, have increased. What is more controversial is whether some populations (for instance Japanese women) are experiencing a shift to the right of the survival curve where the modal age at death has increased, but without a compression, indicating many more people reach a very advanced age and burst through the mortality “wall” instead of squashing against it. This has a very significant implication for the number of very advanced elderlies, and it implies significant population mortality improvement even at advanced ages. Results are still mixed on whether this is really happening at this time.1
Another area of controversy revolves around whether there is compression of morbidity. Will the extra years of life gained by medical progress be spent in an unhealthy disabled state? As is often the case, a good definition is key to understanding the issue. Are we talking about fewer visits to healthcare settings, feeling in better health or less disability?2 They do not necessarily move in tandem. People do not seem to be less sick but seem to be less disabled at a similar age.3
Here once again the extremely old seem to suggest special insights. Teams led by Nir Barzilai and Tom Perls, both of whom presented at past Society of Actuaries’ Living to 100 Symposiums, conducted a study comparing two populations of centenarians to their younger peers for the onset of cancer, cardiovascular disease, diabetes mellitus, hypertension, and osteoporosis. The age at which 20% of the centenarian cohorts was delayed by about two decades compared to their younger peers.4
A small study looking at a composite of health based on a combination of questionnaires, objective tests (such as the “Timed Up and Go” mobility test and the MMSE measuring cognition), as well as the ability to perform IADL (Instrumental Activity of Daily Living) had an equally amazing finding. It found that among the small group of 13 survivors now aged 96 to 106, eight were still passing the original health criteria!5
In the end, actuaries and others have two reasons to be optimistic: More people are living longer as the compression of the mortality curve, or its shift to the right, shows - and, tantalizingly, extended life is not just an addition of only unhealthy years.
Endnotes
- Contrast Robine 2017 vs. Janssen 2019. “Worldwide demography of centenarians,” Jean-Marie Robine, Sarah Cubaynes, Mechanisms of Ageing and Development, www.elsevier.com/locate/mechagedev. “The timing of the transition from mortality compression to mortality delay in Europe, Japan and the United States,” Fanny Janssen and Joop de Beer, Genus (2019) 75:10, https://doi.org/10.1186/s41118-019-0057-y.
- “Is the Compression of Morbidity a Universal Phenomenon?” Jean-Marie Robine, Siu Lan K. Cheung, Shiro Horiuchi and A. Roger Thatcher; Presented at SOA’s Living to 100 and Beyond Symposium, Orlando, FL, January 7-9, 2008. See for more extensive discussion.
- “Compression of Morbidity and Mortality: New Perspectives,” Dept. of Health & Human Services, HHS Public Access, Author manuscript, available in PMC 2017 October 04; Published in final edited form as: N Am Actuar J. 2016 ; 20(4): 341-354. doi:10.1080/10920277.2016.1227269.
- “Compression of Morbidity is Observed Across Cohorts with Exceptional Longevity,” Dept. of Health & Human Services, HHS Public Access, Author manuscript; available in PMC 2017 August 01; Published in final edited form as: J Am Geriatr Soc. 2016 August; 64(8): 1583-1591. doi:10.1111/jgs.14222.
- “10-year follow-up of the Super-Seniors Study: compression of morbidity and genetic factors,” Tindale et al., BMC Geriatrics 2019, https://bmcgeriatr.biomedcentral.com/articles/10.1186/s12877-019-1080-8.




