-
Property & Casualty
Property & Casualty Overview

Property & Casualty
We offer a full range of reinsurance products and the expertise of our talented reinsurance team.
Expertise
Publication
Florida Property Tort Reforms – Evolving Conditions
Publication
Is Human Trafficking the Next Big Liability Exposure for Insurers?
Publication
When Likes Turn to Lawsuits – Social Media Addiction and the Insurance Fallout
Publication
Generative Artificial Intelligence and Its Implications for Weather and Climate Risk Management in Insurance
Publication
Engineered Stone – A Real Emergence of Silicosis
Publication
Who’s Really Behind That Lawsuit? – Claims Handling Challenges From Third-Party Litigation Funding -
Life & Health
Life & Health Overview

Life & Health
We offer a full range of reinsurance products and the expertise of our talented reinsurance team.

Publication
Understanding Physician Contracts When Underwriting Disability Insurance
Publication
Voice Analytics – Insurance Industry Applications [Webinar]
Publication
GLP-1 Receptor Agonists – From Evolution to Revolution U.S. Industry Events
U.S. Industry Events
Publication
Always On: Understanding New Age Addictions and Their Implications for Disability Insurance
Publication
Dying Gracefully – Legal, Ethical, and Insurance Perspectives on Medical Assistance in Dying -
Knowledge Center
Knowledge Center Overview

Knowledge Center
Our global experts share their insights on insurance industry topics.
Trending Topics -
About Us
About Us OverviewCorporate Information

Meet Gen Re
Gen Re delivers reinsurance solutions to the Life & Health and Property & Casualty insurance industries.
- Careers Careers
Underwriting Epilepsy in Life and Disability Insurance

December 07, 2016
Dr. John O’Brien
English
Español
Epilepsy is not a rare condition and traditionally patients with this disease have attracted a certain social stigma. Indeed it has even been suggested that the social stigma associated with epilepsy can be worse than the condition itself. Fortunately, as a result of advocacy groups including support from prominent personalities and sportsmen with epilepsy, this situation is improving. Most underwriters will come across clients with epilepsy. It has been well documented that people with epilepsy have a higher mortality than the normal population. This is due to a number of factors but, as has been emphasised, a certain proportion of the excess mortality is related to the comorbid conditions that often accompany the disease.
Mortality in epilepsy
Some well-conducted prospective studies look at mortality in epilepsy. Lindsten et al. recruited 107 subjects with newly diagnosed epilepsy and followed them for ten years. The standard mortality ratio (SMR) was significantly increased at 2.5. The high mortality risk was particularly evident during the first two years after diagnosis and was most pronounced when the seizures occurred before the age of 60 years.1 They also found that the increased mortality occurred in patients with remote symptomatic epilepsy but not idiopathic epilepsy.
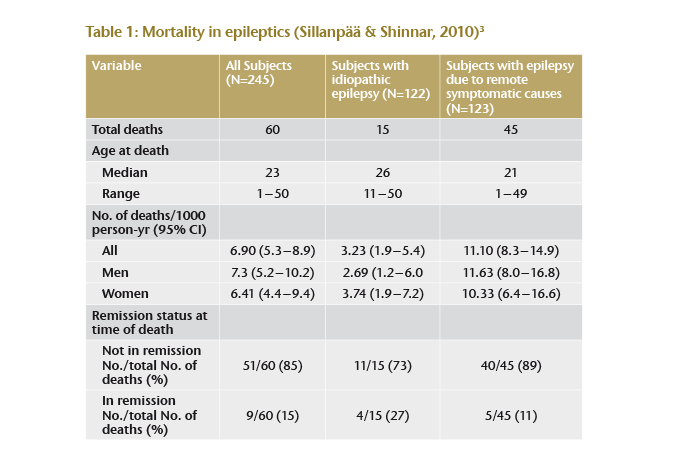
In 2010 Sillanpää et al. followed a cohort of 245 children with a diagnosis of epilepsy for 40 years. It is surprising that a high autopsy rate was achieved with an accurate diagnosis of cause of death in most subjects. In total 24% of the group died, which was three times as high as the expected age and sex-adjusted mortality in the general population. The study generated interesting data regarding the risk factors for mortality. A remote symptomatic cause of epilepsy (i. e. major neurological impairment or insult) was associated with an increased risk of death compared with the idiopathic or cryptogenic epilepsy (37% vs 12%). Approximately half the deaths were directly related to epilepsy, including sudden unexplained death (SUDEP) recorded as the cause in 30% of the deaths. A smaller portion of the deaths, 15%, was associated with seizures and 10% of the deaths were due to accidental drowning.2
It is interesting to note that some of the deaths occurred in subjects who were in remission from their epilepsy (see Table 1). Of these, some were receiving medication and others were not. Deaths not related to epilepsy included pneumonia (mostly in those with remote symptomatic causes) cardiovascular disease and suicide. SUDEP occurred in both groups although it was more common in the subjects with remote symptomatic cause for epilepsy (6 vs 20).
Sudden unexpected death (SUDEP)
Sudden unexpected or unexplained death in epilepsy (SUDEP) accounts for 7% to 17% of deaths. As the name suggests, the reason for these deaths is unclear; however, a number of associations have been identified: SUDEP is more common in young, male epileptics between 20 and 40 years of age, tends to occur at night and is associated with poor seizure control. Indeed, some events may be the result of unwitnessed seizures (though status epilepsy is excluded). Variable associations with antiepileptic medications have been identified but evidence does indicate that patients on multiple drugs are at high risk. But this may be a marker of severity rather than a drug effect. Well-controlled, seizure-free epileptics don’t seem to have an increased SUDEP risk. This is supported by the fact that following successful epilepsy surgery in adults with refractory partial epilepsy, the unexplained death rates are significantly lower in those who achieve seizure freedom.4,5
Suicide
Perhaps surprisingly, one important cause of death in patients with epilepsy is suicide – about 11% or more of deaths can be attributed to suicide. This is more than a tenfold higher prevalence than in the general population. The link between epilepsy and suicide is not well understood. Experimental findings if this is related to depression have been contradictory – although the incidence of depression is certainly higher in epileptics than in non-epileptics. Up to a third of patients with epilepsy who had suicidal ideation had either no or only mild depressive symptoms. Anti-epileptic drug therapy has been considered another cause. There are conflicting reports and a large meta-analysis was not able to show a clear relationship.6 Risk factors for suicidal behaviour in epileptics include psychiatric comorbidity, temporal lobe epilepsy, female gender and early-onset epilepsy. One theory is that interictal dysphoric disorder may be associated with suicidal thoughts. While it has been suggested that suicide is more common in patients with severe epilepsy, it has also been reported in patients that have recently achieved complete seizure freedom and excellent epilepsy control.
Accidental death
Accidental death is predictably increased in the epileptic population. This can result from injury at the time of seizure or from the seizure precipitating a motor vehicle or other accident. There is an increased risk of drowning, which can occur even in the bath. Aspiration pneumonia following a seizure is a cause of death most commonly associated with comorbid neurological disease. In a large study by Kwon over 10,000 individuals with epilepsy were compared with 40,000 individuals without. After adjustment for medical and psychiatric comorbidities there was no increased incidence of suicide or motor vehicle accident but epileptic patients were more likely to be assaulted.7
Morbidity in epilepsy
Clients with epilepsy may also apply for other insurance products than Life insurance, including Disability insurance. Underwriting this type of insurance should be approached with caution. Seizures, particularly uncontrolled ones and status epilepsy (continuous seizures), can result in cerebral hypoxia with resultant permanent neurological impairment. Accidents precipitated by a seizure can also result in significant injury and impairment.
Epilepsy patients generally tend to have more physical problems related to seizures (e. g. fractures and bruising). Important to note is that the stigma surrounding epilepsy and the associated social discrimination can lead to increased rates of depression and anxiety. The unpredictability of seizures can impact a patient’s quality of life and decrease their self-esteem.
Occupation, of course, will be an important consideration. Occupations that involve working with machinery, working at heights or in hazardous conditions are especially dangerous for epileptics. For example, epileptics in occupations that require a vocational licence or where driving is essential are at increased risk of disability. A single epileptic fit will result in the withdrawal of an individual’s licence, and a public service or heavy goods vehicle licence may be permanently revoked. Occupational health regulations will preclude epileptics from working in an environment in which their seizures could be potentially harmful to themselves or others.
Underwriting recommendations
When underwriting a client with epilepsy, it is necessary to assess all the factors that can contribute to the increased morbidity and mortality in this group.
- Initially, it is important to determine whether the epilepsy is idiopathic or associated with other neurological or psychiatric conditions. Most clients will have had neuroimaging and this should be adequate to exclude serious independent diseases, such as brain tumours and degenerative brain conditions.
- Next, one needs to establish the type of seizure, as risk of death is related to type and severity of seizure, with simple and partial seizures being much less dangerous than seizures associated with grand mal features (tonic-clonic contractions with loss of consciousness).
- It is then important to look at the level of control. Clients who have well-controlled epilepsy, and who have been seizure-free for a number of years, pose a much lower threat of increased mortality than clients with poorly controlled epilepsy and ongoing seizures.
- The medication needs to be assessed. Where requirements for treatment include multiple drugs, the likelihood of poor control and breakthrough seizures increases.
- Following successful surgical intervention, cure can be achieved and mortality can be similar to the non-epileptic population.
- Risks of seizures during specific occupations need to be considered, but generally the client’s occupation will have been determined by the presence of the epilepsy unless it is of fairly late onset.
- Before thinking of disability insurance, the client needs to have been seizure-free for at least five years, have a normal CT or MRI and have no other history of concern, including assessment of seizure type. If possible, one should consider excluding impairment of the central nervous system (CNS) as this would be the most likely consequence of a severe or uncontrolled seizure.
While epilepsy may be fairly common, it has a wide spectrum of severities and presentations. This means that each client must be carefully and individually assessed.





