-
Property & Casualty
Property & Casualty Overview

Property & Casualty
We offer a full range of reinsurance products and the expertise of our talented reinsurance team.
Expertise
Publication
Biometric Information Privacy – Statutes, Claims and Litigation [Update]
Publication
Inflation – What’s Next for the Insurance Industry and the Policyholders it Serves?
Publication
Human Activity Generates Carbon and Warms the Atmosphere. Is Human Ingenuity Part of the Solution?
Publication
Illinois Changes Stance on Construction Defect Claims – The Trend Continues
Publication
Generative Artificial Intelligence in Insurance – Four Aspects of the Current Debate
Publication
Battered Umbrella – A Market in Urgent Need of Fixing -
Life & Health
Life & Health Overview

Life & Health
We offer a full range of reinsurance products and the expertise of our talented reinsurance team.

Publication
Underwriting High Net Worth Foreign Nationals – Considerations for U.S. Life Insurance Companies
Publication
Group Term Life Rate & Risk Management – Results of 2023 U.S. Survey
Publication
Trend Spotting on the Accelerated Underwriting Journey
Publication
All in a Day’s Work – The Impact of Non-Medical Factors in Disability Claims U.S. Industry Events
U.S. Industry Events
Publication
Marginal Gains in the Medicare Supplement Market -
Knowledge Center
Knowledge Center Overview

Knowledge Center
Our global experts share their insights on insurance industry topics.
Trending Topics -
About Us
About Us OverviewCorporate Information

Meet Gen Re
Gen Re delivers reinsurance solutions to the Life & Health and Property & Casualty insurance industries.
- Careers Careers
Melanoma Monday – an Update on Skin Cancer Claims

November 20, 2015
Mary Enslin
English
Monday 4 May, 2015 was Melanoma Monday, a day created by the American Academy of Dermatology to increase awareness of Melanoma and other types of skin cancer. As you can imagine not many cancers are “special” enough to get their own day, so what is it about Melanoma that makes it so notorious?
Skin cancer is the most common type of cancer – over the past three decades more people have had skin cancer than all other cancers combined. However, due to the fact that they are usually not disabling or fatal, skin cancers are routinely excluded from cancer statistics. Melanoma is the exception – while it is the least common type of skin cancer, it is often called the most dangerous, accounting for up to 75% of all skin cancer fatalities. To put it simply, one person dies of Melanoma every hour.
Definition
Melanoma can be described as the uncontrolled growth or multiplication of pigment-containing skin cells (melanocytes) resulting in the formation of malignant tumors. This growth is caused when irreparable damage occurs to the DNA of skin cells, most often as a result of ultraviolet radiation from sunshine or tanning beds. While Melanoma occurs most commonly on the skin, it can also develop in other areas of the body where melanocytes are present, such as the eyes, underneath nails and inside the nose and mouth.
Epidemiology
Rates of both non-Melanoma and Melanoma have been rising for at least 30 years. In fact, of the seven most common cancers in the US, Melanoma is the only one with an increasing incidence. Currently, one in three cancers diagnosed is a skin cancer and the American Cancer Society estimates more than 135,000 new cases are diagnosed in the US each year – in 2015 an estimated 73,870 of these (more than half) will be invasive and almost 10,000 (7%) will be fatal. It is further estimated that on average 2.1% of adults worldwide will be diagnosed with Melanoma of the skin at some point during their lifetime. However, the risk for each person can be affected by a number of different factors, including:
- Complexion – Melanoma is 20 times more common in individuals with fair skin, freckling and light hair. 1 in 40 fair-skinned adults will develop Melanoma.
- Age – the average age at when Melanoma is detected is 62 years, but it is not uncommon to find it in those younger than 30. In fact, it is the most common cancer in young adults (25-29 years) and the second most common cancer for young people (15-29 years).
- Ultraviolet light exposure – some studies estimate that just five sunburns in a lifetime doubles an individual’s risk of developing Melanoma. Five sunburns may sound like many, but the Skin Cancer Foundation conducted a poll that showed 42% of people sunburn at least once a year.
- Family or personal history – survivors of Melanoma are approximately nine times as likely as the general population to develop a new Melanoma.
- Geographical location – because of the association with skin colour and ultraviolet exposure Melanoma is particularly common in northern Europeans and northwestern Europeans living in sunny climates. Oceania, North America, Europe, Southern Africa and Latin America have higher rates than elsewhere.

Symptoms and Diagnosis
The most common early signs of Melanoma include a mole that is either growing in size, unusual looking, does not look like any other mole, non-uniform (has an odd shape or uneven colour). This may be accompanied with itching, swelling, tenderness or pain. In women the most common site is the legs, and in men the back. Early signs of Melanoma are summarized by the mnemonic ABCDE (see Figure 2).

Metastatic Melanoma may cause non-specific symptoms including nausea, weight-loss, vomiting, fatigue, loss of appetite, dizziness, etc.
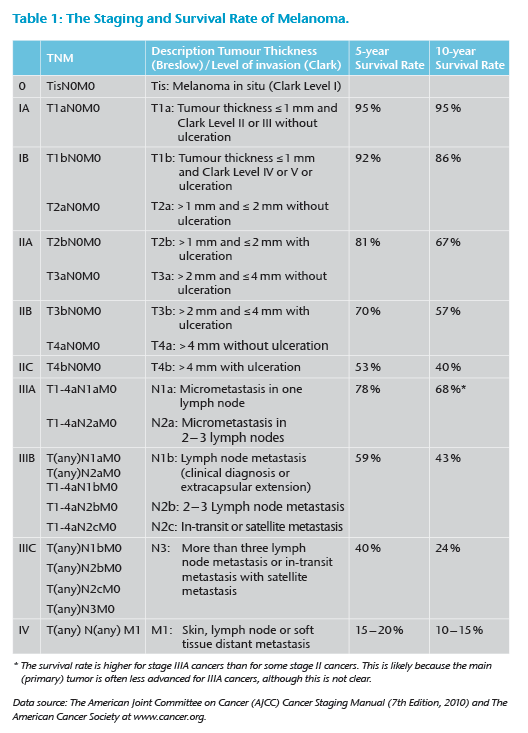
Diagnosis is based on warning signs and confirmed with either punch, excisional or incisional biopsy. The stage of the cancer is then determined based on the tumour thickness (Breslow score) and level of invasion (Clark score), as well as other factors, such as whether ulceration is present, mitotic rate, and the degree of lymph node involvement. If the Melanoma is found to be advanced certain imaging tests will be performed and biopsy samples may be tested to see if the cells have mutations in the BRAF gene, as approximately half of all Melanomas have this mutation.
Treatment
A number of treatment options exist, depending on the stage of the Melanoma and other individual circumstances, but generally treatment options may include:
- Surgery
- Immunotherapy
- Targeted therapy
- Chemotherapy
- Radiation therapy.
A number of advances in pharmacotherapy research are exploring new treatment possibilities for unresectable or metastatic Melanoma. Areas of research include combination therapies, such as dabrafenib and trametinib; gene therapy targeted at the MITF, MEK and BRAF genes; melanin synthesis, adoptive cell therapy (ACT) using immune cells isolated from a patient‘s own Melanoma tumor, vaccines that train the immune system to fight cancer, and the use of oncolytic viruses.
Prognosis
If recognised and treated early, Melanoma is almost always curable with little or no residual impairment. However, if allowed to develop it is an aggressive cancer that advances quickly and spreads to other parts of the body. At this stage it is difficult to treat and can be fatal. Brain metastases are particularly common in patients with metastatic Melanoma. It can also spread to the liver, bones, abdomen or distant lymph nodes.
The overall 5-year survival rate for patients whose Melanoma is detected early, before the tumor has spread to regional lymph nodes or other organs, is usually high – above 90%. When there is distant metastasis, the cancer is generally considered incurable. The five-year survival rate is less than 20% and median survival is 6-12 months. At this stage treatment is palliative, focusing on life extension and quality of life.
Melanoma and Claims
A report by Cancer Research UK indicated that while the mortality rate of Melanoma has remained relatively stable (approximately 2.5 cases per 100,000 ), the number of new cases being diagnosed has risen steadily over the past 20 years – from just under 15 per 100,000 cases in 1992 to over 20 per 100,000 cases in 2012. From this we can defer that the rising incidence of Melanoma will have a more significant effect on disability and critical illness claims experience than mortality.
Critical illness
Critical illness (CI) insurance was first introduced with the intention of providing benefits to individuals who suffered a life-threatening event. Historically, cancer was associated with high mortality and morbidity and as such formed one of the cornerstones of any CI product (typically alongside heart attack, stroke and coronary artery bypass grafting). However, medical advances, increased awareness and the roll-out of screening programs have resulted in more and more cancers being detected at an early stage. Thus many previously life threatening cancers are being treated successfully with relatively little disruption to the patient’s life.
Combined with this is the evolution of the CI product to include different levels of payment according to the severity of the condition claimed. Essentially, products that previously only paid 100% of the benefit for severe cancers could now pay 50% or 25% for less severe, earlier detected cancers.
Further, exclusions for early stage cancers, especially skin cancers, are becoming increasingly lenient. Considering that cancer is frequently the leading cause of CI claims in both males and females, claims assessors need to be aware of how changes in medical technology and in CI product design will affect claims experience.
Melanoma is a good example of one such cancer and claims assessors should consider the following when assessing skin cancer claims:
- The histology and staging – detailed information regarding the staging will be particularly relevant to distinguish Melanoma from other skin cancers (many of which are explicitly excluded) and from pre-cancerous conditions.
- The policy wording – depending on the market, many CI products have specific exclusions pertaining to skin cancers and early stage cancers.
- Non-disclosure and misrepresentation investigations – it may be difficult to determine whether a Melanoma existed prior to the claimant taking out the policy as a mole may have been present for many years, but the claimant may not have been aware of it or may not have considered this worth disclosing. Again, there may be some differences across markets, but generally the test for material non-disclosure or misrepresentation is whether a person imbued with common knowledge would believe that the disclosed information would have an impact on whether an insurer would accept the risk or not. If a person believed a mole or skin lesion to be benign, or had been told “not to worry” by a doctor, then it would not be reasonable to expect them to disclose the presence of the mole and there would be no case for non-disclosure.
Disability products
It would be a mistake to think that a rise in Melanoma claims will only affect CI products. A 2014 study in the US found that the estimated annual productivity losses attributable to Melanoma totaled $2.85 billion. As mentioned, the severity and location of the Melanoma will determine the treatment options available. Early Melanomas will frequently be treated with surgery and perhaps a short course of chemotherapy or radiation. This will likely result in short-term temporary income protection claims only.
However, more advanced Melanomas will likely require extensive treatment, resulting in potential long-term income protection claims. Where there is distant metastases treatment will be palliative in nature and insurers can expect to see lump sum disability and even terminal illness claims.
One challenge faced when assessing disability claims due to cancer is determining the permanence of the claimant’s condition. As treatment can often span over years, with responses varying between individuals, doctors may be reticent to comment on prognosis. This is further complicated by the fact that the treatment itself is often more disabling than the cancer. These factors need to be taken into consideration when assessing claims.
Conclusion
While skin cancer is common, the relatively harmless nature of most skin cancers means that most individuals will not have any serious health consequences as a result. Melanoma is the exception – an aggressive and serious cancer that frequently results in disability and death if not treated early. As the incidence of Melanoma cases continues to rise, insurers can expect to see an increase in claims across benefits. Where there is advanced disease, deciding on the validity of these claims may be fairly straightforward. However, where Melanoma is detected early claims assessors need to consider a number of factors. The case study following illustrates some of the challenges highlighted in this article.





