-
Property & Casualty
Property & Casualty Overview

Property & Casualty
We offer a full range of reinsurance products and the expertise of our talented reinsurance team.
Expertise
Publication
Production of Lithium-Ion Batteries
Publication
Time to Limit the Risk of Cyber War in Property (Re)insurance
Publication
Generative Artificial Intelligence in Insurance – Three Lessons for Transformation from Past Arrivals of General-Purpose Technologies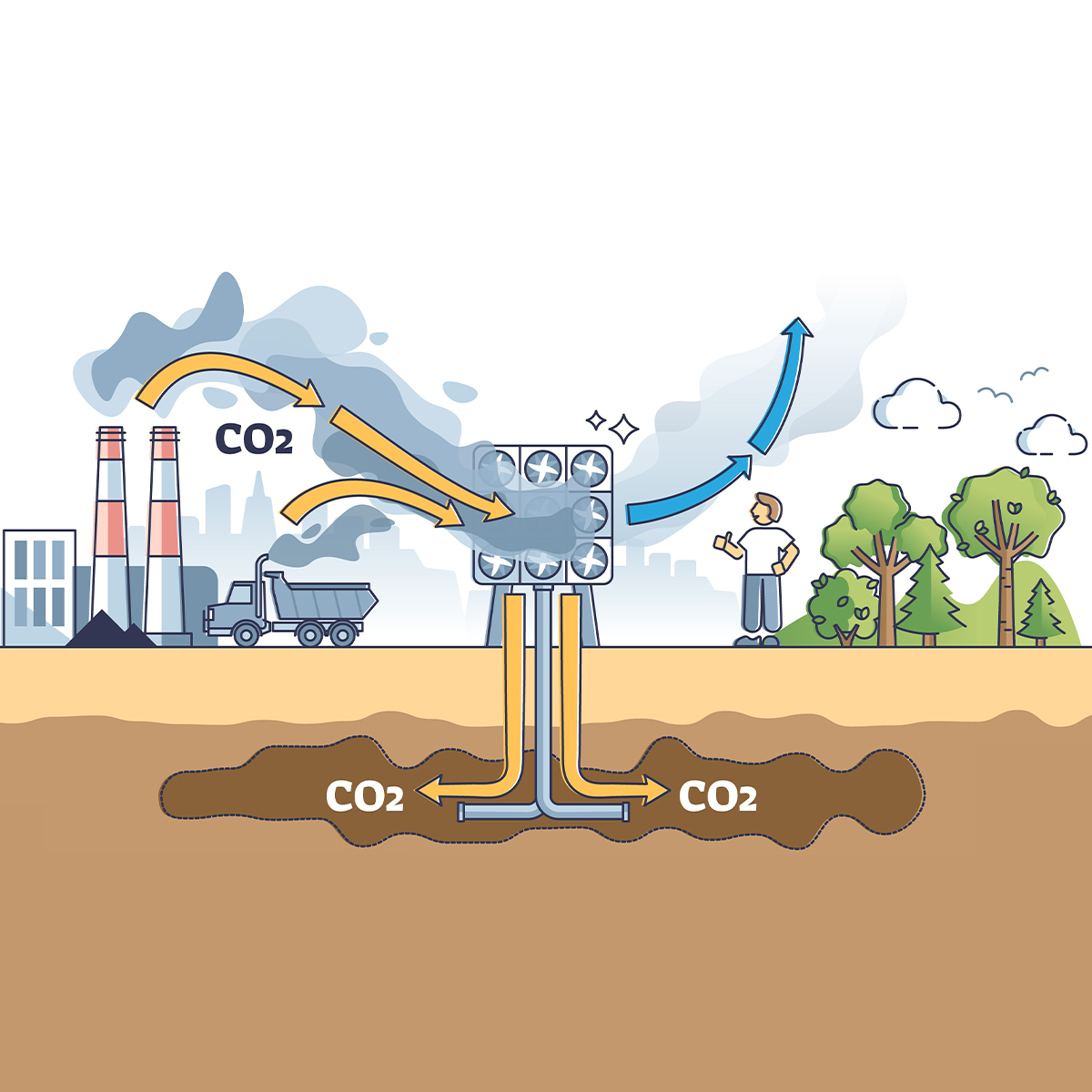
Publication
Human Activity Generates Carbon and Warms the Atmosphere. Is Human Ingenuity Part of the Solution?
Publication
Inflation – What’s Next for the Insurance Industry and the Policyholders it Serves? -
Life & Health
Life & Health Overview

Life & Health
Gen Re’s valuable insights and risk transfer solutions help clients improve their business results. With tailor-made reinsurance programs, clients can achieve their life & health risk management objectives.
UnderwritingTraining & Education
Publication
The Key Elements of Critical Illness Definitions for Mental Health Disorders
Publication
What Are We to Make of Cannabis Use in The Insured Population? Business School
Business School
Publication
Knife or Needle: Will the New Weight Loss Medication Replace Bariatric Surgery?
Publication
Weight Loss Medication of the Future – Will We Soon Live in a Society Without Obesity? Moving The Dial On Mental Health
Moving The Dial On Mental Health -
Knowledge Center
Knowledge Center Overview

Knowledge Center
Our global experts share their insights on insurance industry topics.
Trending Topics -
About Us
About Us OverviewCorporate Information

Meet Gen Re
Gen Re delivers reinsurance solutions to the Life & Health and Property & Casualty insurance industries.
- Careers Careers
Ushering in a New Era of Cystic Fibrosis Management

May 06, 2024
Dr. Chris Ball
English
There has been dramatic change in the management of many medical conditions over the last 10 years, none more so than cystic fibrosis. There has been improvement in the day-to-day lives of many people who experience the illness, their general health and prognosis.
The improvements in lived experience for those experiencing cystic fibrosis are driven by significant advances in the treatment of “downstream” problems (e.g. mucus accumulation and respiratory tract infections) and also in medications that influence the fundamental molecular defects of the illness. Cystic fibrosis is genetically determined by variants in an autosomal recessive gene, called the cystic fibrosis transmembrane conductance regulator (CFTR) gene, that influences the balance between water and electrolytes on the surface of many organs. Classically these are the lungs, but also the intestine, pancreas (80% of people affected), biliary tree, cervix, vas deferens and sweat glands.
A huge number of variants of the gene have been described, about 700 of which are disease-causing. These many variants influence the protean nature of the problem, ranging from the very severe to the relatively mild.1
The incidence is approximately 1 in 3,500 live births but can vary greatly by region. There is a lack of reliable data from many parts of the world.2 The diagnosis is usually made early in life when a child fails to thrive or experiences respiratory problems. Others are identified later in life when the problem is limited to a single organ, such as the pancreas, or is found to be the underlying cause for infertility.
A number of neonatal screening programmes are now underway with the potential for earlier intervention and subsequent improvement of mortality. Where there is significant clinical suspicion, the gene can be sequenced as the older diagnostic test, the sweat test, is recognised as not necessarily ruling out the diagnosis.3
Treatment with the newer drugs (CTFR modulators) is highly effective but costly. A “personalised medicine” approach is increasingly used to identify the best combination of modulators for each individual. Early intervention is advised. The drug is licensed in the U.S. for children from the age of two, and in the UK licences have recently been extended to children between two and five years of age. However, the UK National Institute for Clinical Excellence has published draft guidelines concluding that, despite the effectiveness of the treatments, they were too expensive to be recommended for National Health Service use in England.4 Understandably this has led to significant concern among people with the disorder and especially parents of children living with the illness.5
In addition to improvements in the lungs, medications are able to prevent or delay the onset of pancreatic insufficiency, which has led to a reduction in the incidence of cystic fibrosis diabetes. The longer-term effects on other organs such as the liver and related complications (e.g. bone and renal problems or prolonged antibiotic use), have yet to be fully appreciated.6
Impressive as the outcomes are for medication, improvements in physical therapies to reduce mucus build‑up also have a significant role to play in preventing deterioration in lung function. Inhaling mucolytic drugs has been shown to be of benefit but their long-term role in the era of CTFR modulators may change.
Prevention of infection through means such as vaccination is important but cannot entirely prevent acute exacerbations or chronic infections which require energetic management. For those who have severe lung disease, transplantation remains an option. The hope is that this will become a much rarer intervention with the widespread use of CTFR modulators. These alternative developments are vital for people who are ineligible for, or have no benefit from, the CTFR modulators. By extrapolation these other interventions may be of benefit in other chronic lung conditions (e.g. bronchiectasis and chronic obstructive pulmonary disease [COPD]). In their paper in The Lancet, Perrem and Ratjen have highlighted other developing therapeutic avenues for cystic fibrosis, such as gene‑editing.7
Cystic fibrosis has long been thought of as a paediatric disorder but has become a chronic disease to be managed into adulthood. The increasing sophistication and cost of management is likely only to increase the inequality of outcome between those who have good access to care and those who do not.
New treatments for those with the most common genetic variant have been predicted to increase the estimated median age of survival by 6.1 years. Survival with early initiation and persistence of treatment is predicted to be a more impressive 17.7 years, if the treatment is started at age six, but only 3.8 years if it is started at age 25.8
The median survival in the new era has been reported as “close to 50 years” and is likely to increase with time. Another way of looking at this is the prediction that the adult population with cystic fibrosis will double in the next 20 years.9
A “new era” in cystic fibrosis care has been announced but with the caveat “always changing, always adapting”. The new treatments are not universally effective, bringing potential side-effects and the challenge of the unknowns of long-term use of new medications. It is of concern that these striking innovations will not be available or affordable across all markets.
Individuals will vary significantly as to when in the course of their illness they are able to access the therapies, if at all. Individual consideration will remain the cornerstone of underwriting for the foreseeable future. Nevertheless, the picture is a largely positive one and a change in approach is required from insurers who will be increasingly challenged to offer fair rates to a growing number of adults living with cystic fibrosis.10
- The New England Journal of Medicine, Grasemann, H.; et al Cystic Fibrosis, https://www.nejm.org/doi/pdf/10.1056/NEJMra2216474?articleTools=true
- National Library of Medicine, Guo, J.; et al Worldwide rates of diagnosis and effective treatment for cystic fibrosis, https://pubmed.ncbi.nlm.nih.gov/35125294/
- National Library of Medicine, Grosse, S.D.; et al Potential impact of newborn screening for cystic fibrosis on child survival: a systematic review and analysis, https://pubmed.ncbi.nlm.nih.gov/16939748/
- Medscape UK, Russell, P. Cystic Fibrosis Drugs Licensed for Use in Younger Children, https://www.medscape.co.uk/viewarticle/cystic-fibrosis-drugs-licensed-use-younger-children-2023a1000sn8?ecd=wnl_ret_231116_mscpmrk-GB_daily_etid6063131&uac=117244AK&impID=6063131&sso=true
- The Times, Templeton, S.‑K.Cystic fibrosis sufferers denied life-prolonging drug by NHS, https://www.thetimes.co.uk/article/cystic-fibrosis-sufferers-denied-life-prolonging-drug-by-nhs-w062qc5z3
- Ibid, see endnote 1
- The Lancet, Perrem, L.; et al Are we there yet? The ongoing journey of cystic fibrosis care, https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(23)01727-0/abstract
- Rubin, J.L.; et al Modeling long-term health outcomes of patients with cystic fibrosis homozygous for F508del‑CFTR treated with lumacaftor/ivacaftor. Ther. Adv. Respir. Dis. 2019, 13, 1‑23
- MDPI, Scotet, V.; et al The Changing Epidemiology of Cystic Fibrosis: Incidence, Survival and Impact of the CFTR Gene Discovery, https://www.mdpi.com/2073-4425/11/6/589
UpToDate, Cystic fibrosis: Clinical manifestations and diagnosis, https://www.uptodate.com/contents/cystic-fibrosis-clinical-manifestations-and-diagnosis?search=cystic%20fibrosis%20prognosis&source=search_result&selectedTitle=3~150&usage_type=default&display_rank=3
The Lancet, Taylor‑Cousar, J.L.; et al CFTR modulator therapy: transforming the landscape of clinical care in cystic fibrosis, https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(23)01609-4/abstract - Lippincott, Diener, B.; et al Current Opinion in Pediatrics, A new era in cystic fibrosis care: always changing and adapting, https://journals.lww.com/co-pediatrics/abstract/2023/10000/a_new_era_in_cystic_fibrosis_care__always_changing.14.aspx
All endnotes last accessed on 28 February 2024.




