-
Property & Casualty
Property & Casualty Overview

Property & Casualty
We offer a full range of reinsurance products and the expertise of our talented reinsurance team.
Expertise
Publication
Production of Lithium-Ion Batteries
Publication
Time to Limit the Risk of Cyber War in Property (Re)insurance
Publication
Generative Artificial Intelligence in Insurance – Three Lessons for Transformation from Past Arrivals of General-Purpose Technologies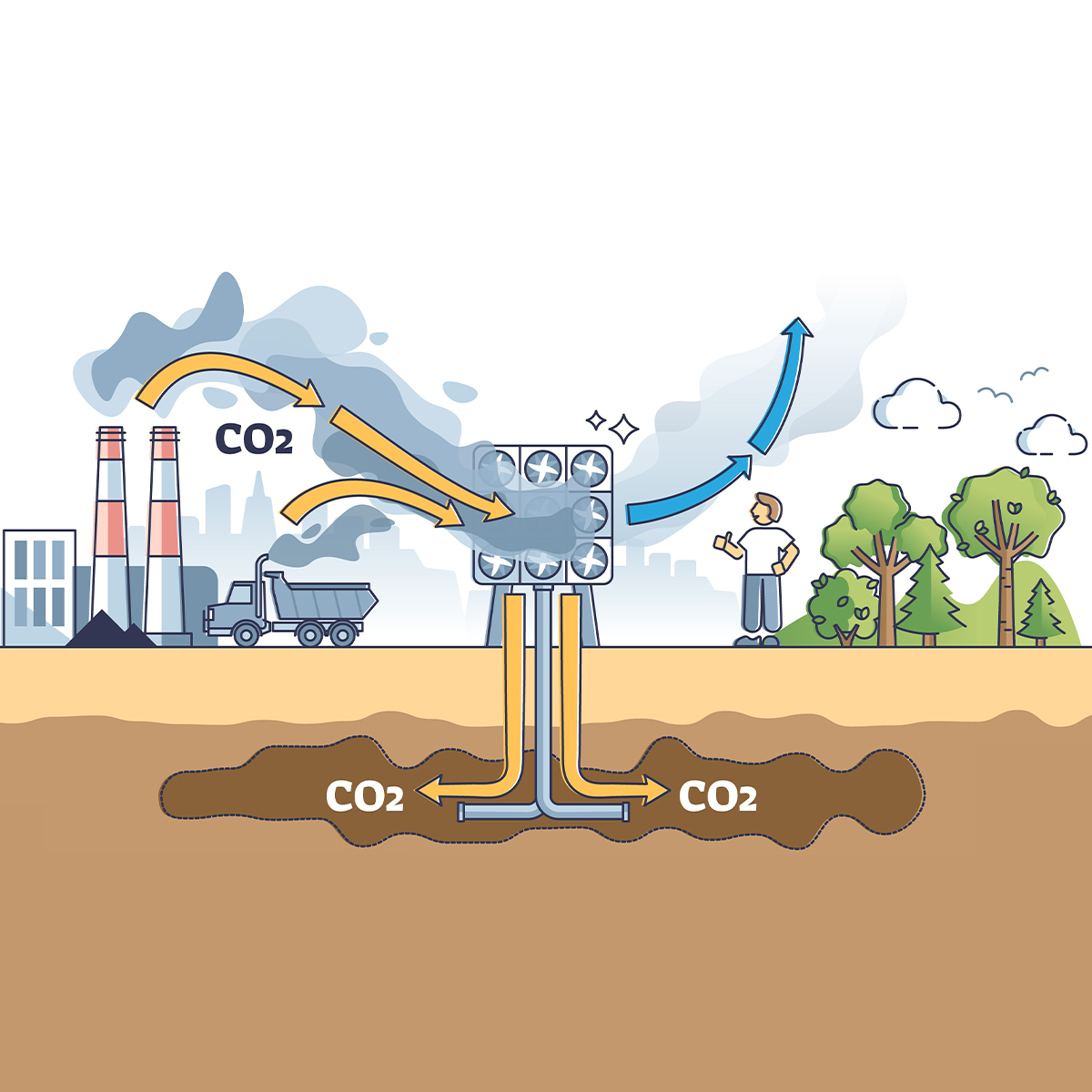
Publication
Human Activity Generates Carbon and Warms the Atmosphere. Is Human Ingenuity Part of the Solution?
Publication
Inflation – What’s Next for the Insurance Industry and the Policyholders it Serves? -
Life & Health
Life & Health Overview

Life & Health
Gen Re’s valuable insights and risk transfer solutions help clients improve their business results. With tailor-made reinsurance programs, clients can achieve their life & health risk management objectives.
UnderwritingTraining & Education
Publication
The Key Elements of Critical Illness Definitions for Mental Health Disorders
Publication
What Are We to Make of Cannabis Use in The Insured Population? Business School
Business School
Publication
Knife or Needle: Will the New Weight Loss Medication Replace Bariatric Surgery?
Publication
Weight Loss Medication of the Future – Will We Soon Live in a Society Without Obesity? Moving The Dial On Mental Health
Moving The Dial On Mental Health -
Knowledge Center
Knowledge Center Overview

Knowledge Center
Our global experts share their insights on insurance industry topics.
Trending Topics -
About Us
About Us OverviewCorporate Information

Meet Gen Re
Gen Re delivers reinsurance solutions to the Life & Health and Property & Casualty insurance industries.
- Careers Careers
A Digital Solution for Income Protection Claims

May 02, 2019
Ross Campbell
English
New technologies mean Disability Income Protection (IP) claims managers can enhance and expand the support and services they offer. Digital solutions can also be used to enhance and improve the claims experience. TrackActive is a company that has developed an artificial intelligence-driven engagement platform that provides early, cost effective and scalable interventions for rehabilitation and prevention of musculoskeletal conditions and other chronic disease. To find out more, I spoke with TrackActive co-founder and CEO Michael Levens.
RC: What is it that drew you to the Disability insurance business?
ML: We launched a product called TrackActive Pro. It links up patients with musculoskeletal conditions to clinics and physiotherapists. People using our service to support insurance claims suggested we go direct to insurers. They said it would reduce the friction they felt in making and processing their claims – the form filling and episodic, ongoing interactions with the insurer. So, we developed a fully digital sister product called TrackActive Me.
RC: Have you encountered any challenges so far?
ML: Disability carriers don’t own the physiotherapist or the health professional, they just buy services from them, so how we get our product into the insurance value chain is very important. Insurers already have excellent claims management processes. However, these rely heavily on paper, which means we have to show that our digital offering can add value or even improve upon them.
RC: What are the benefits of TrackActive Me to the IP insurer and for the claimant?
ML: Engaging health professionals comes with a cost and it’s ongoing each time a claimant sits with one to process a claim. The quality and impact of the digitised version of our service compares very favourably; it’s as effective as going to see a health professional and the prescribed exercises can be accessed on demand. The idea of a physiotherapist in your pocket that allows for remote monitoring is a stepping stone towards self-management. If things are working less than optimally, the user can easily opt into seeing a health professional in person, via TrackActive Pro. Blending service and product like this is important.
RC: Must insurers think and act differently to use a digital tool?
ML: Yes, it can be difficult for insurers to visualise a digital version of an analogue process. For a start, TrackActive Me is very self-managed. While we have taken down an implementation barrier by making it simple for claimants to get and to use, we have removed some control of the process, too. Insurers can give the tool to their claimants, or a health professional can bring them on-board after they have gone through their primary treatment.
RC: What is your message to IP insurers who are thinking about digital alternatives?
ML: It’s easy, really. We want to engage with companies willing to see that new digital process are not only capable but will enhance their offering. Companies that want to join the dots between the digital and the analogue. Those that have an open mind to technology and want to look at ways the current model can be enhanced. I’d say to any Income Protection (IP) insurer, set up a pilot or a project to let us demonstrate what TrackActive can do.
The ideal working approach is collaboration to help the technologies of startups mature in ways that fit best to the needs of IP insurers, before plugging them into existing systems by using open application programming interfaces.
Technology will reduce the amount of manual work involved in assessing an IP claim. There are long-term benefits for insurers as well in the rich customer data that will be generated. Analysis of the data will provide predictive intelligence to help deliver better value and service to new claimants. It will help to anticipate claims and give focus to providing effective interventions. Ultimately, IP claims solutions delivered using AI or other digital means will save process costs that can then be passed on to customers in the form of reduced premiums. Meanwhile, a more frictionless and transparent solution to managing customers’ recovery in claim stages will significantly add to customers’ satisfaction.



