-
Property & Casualty
Property & Casualty Overview

Property & Casualty
We offer a full range of reinsurance products and the expertise of our talented reinsurance team.
Expertise
Publication
Use of Artificial Intelligence in Fire Protection and Property Insurance – Opportunities and Challenges
Publication
Public Administrations’ Liability – Jurisprudential Evolution, Insurance Implications, and a Comparative Analysis Across Countries
Publication
Generative Artificial Intelligence and Its Implications for Weather and Climate Risk Management in Insurance
Publication
Engineered Stone – A Real Emergence of Silicosis
Publication
Risk Management Review 2025 -
Life & Health
Life & Health Overview

Life & Health
Gen Re’s valuable insights and risk transfer solutions help clients improve their business results. With tailor-made reinsurance programs, clients can achieve their life & health risk management objectives.
UnderwritingTraining & Education
Publication
Diabetes and Critical Illness Insurance – Bridging the Protection Gap
Publication
Underwriting the Dead? How Smartphones Will Change Outcomes After Sudden Cardiac Arrest
Publication
Always On: Understanding New Age Addictions and Their Implications for Disability Insurance
Publication
Dying Gracefully – Legal, Ethical, and Insurance Perspectives on Medical Assistance in Dying
Publication
AI Agent Potential – How Orchestration and Contextual Foundations Can Reshape (Re)Insurance Workflows Business School
Business School -
Knowledge Center
Knowledge Center Overview

Knowledge Center
Our global experts share their insights on insurance industry topics.
Trending Topics -
About Us
About Us OverviewCorporate Information

Meet Gen Re
Gen Re delivers reinsurance solutions to the Life & Health and Property & Casualty insurance industries.
- Careers Careers
Rheumatoid Arthritis – Advances in Therapy

January 17, 2018
Lyn Franks
English
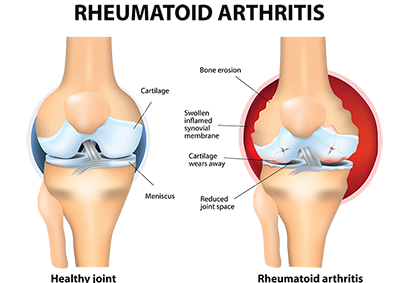
Rheumatoid Arthritis (RA) is an inflammatory autoimmune polyarthritis of unknown aetiology that targets the synovial tissue of moveable joints. It is a member of a class of rheumatic diseases with inflammatory arthritis as a primary symptom, but it may also affect other organs of the body.
The two main classes of RA are seropositive and seronegative RA, which are distinguished by the presence or absence of anti-cyclic citrullinated peptides (anti-CCPs), Seropositive RA has anti-cyclic citrullinated peptides (anti-CCPs), also referred to as anti-citrullinated protein antibodies (ACPAs). Most RA seronegative patients either do not possess these antibodies or possess them at extremely low levels. A diagnosis of seronegative RA is based on characteristic history and clinical findings. Seronegative patients may, however, go on to develop these antibodies many years after their initial diagnosis.1
Whether a person has seropositive or seronegative RA can influence the choice of treatment.2 Advances in therapies and their methods of delivery have markedly improved the outcomes for people diagnosed with RA, and the outlook for sufferers looks even more promising with newer methods of treatments currently under development.
Risk Factors
The specific causes of RA remain unknown, although it is believed that it results from a combination of genetic and environmental factors.3 The following are associated with a higher incidence of RA:
- Ethnicity – Caucasians and Native Americans are at greater risk of developing RA.4
- Family history5
- Gender – RA is more common in females.6
- Obesity – This condition appears to infer an increased risk of RA, especially in females diagnosed with the disease at age 55 or younger.7
- Environmental exposure – Although there is some uncertainly in this area, it appears that some exposures, such as asbestos or silica, may increase the risk of development.8
- Age – While development may occur at any age, RA is most commonly diagnosed in people between the ages of 40 to 60,9 and occasionally at slightly older ages in males.10
- Smoking – A strong risk factor; smoking cessation appears to improve patient outcomes.11
- Periodontal disease (PD) – A chronic inflammatory disease of the gums. The destructive mechanism is similar in PD and RA, as the inflammatory cells and pro-inflammatory cytokines responsible for bone erosion in RA also drive gum disease and tooth destruction in PD. A growing body of research provides increasing evidence of an association between RA and gum disease. The prevalence of PD in patients with RA is more than twofold that of the general population and more severe in patients with RA. Recent findings indicate that infection with the bacterial enzyme p.gingivalis precedes RA.12 However, research has not yet proven a cause and effect, although there is increasing evidence that PD does not always follow the onset of RA, and may even precede it.13 It is essential that patients with both RA and PD follow strict dental hygiene in order to avoid both increased inflammatory response from PD and to prevent tooth loss.
Other Complications
RA is frequently complicated by extra articular manifestations, most commonly in seropositive patients with more advanced joint disease.14 Common examples include the following:15
- Rheumatoid nodules – These usually form around pressure points, such as the elbows, knees and feet but can form anywhere in the body, including the lungs.
- Sjogren’s syndrome – Can result in dry eyes (sicca) and mouth with associated difficulty in swallowing and speaking and lack of tears, leading to drying of the cornea
- Infections – Due to a compromised immune system.
- Lung disease – A major contributor to morbidity and mortality, and includes pulmonary parenchymal disease, pleural thickening and effusions, vasculitis, and pulmonary hypertension.16
- Heart problems – Increased risk of developing atherosclerosis, the most common cardiovascular manifestation in rheumatoid arthritis. Cardiovascular disease is the main cause of death in the RA patient, with the death rate from cardivascualr disease being twice that of the average person. It may also be a complication of treatment.17 A recent study by the Mayo Clinic, however, has recorded a decrease in RA-associated mortality related to heart problems, probably associated with improvements in therapy and increased screening for cardiovascular risk factors.18
- Lymphoma – Potentially induced by the inflammatory nature of RA.
General Principles of Treatment
There is currently no cure for RA. The goals of treatment are to decrease pain and inflammation, retard progression of joint erosions, restore function and achieve remission, and maintain a satisfactory quality of life. Treatments include the following:
- NSAIDs (Nonsteroidal anti-inflammatory drugs) provide relief of pain and stiffness and reduce inflammation. Common short-term side effects include gastric or stomach irritation, a rise in blood pressure, and impaired renal function. Long-term therapy can lead to additional problems, including peptic ulcer and gastrointestinal bleeding, cardiovascular disease, and liver toxicity.19
- Steroids (corticosteroid, including prednisone and prednisolone) reduce inflammation and pain, especially in episodes of an acute exacerbation of symptoms. Long-term use commonly leads to weight gain and may lead to other problems, including bone thinning (osteopenia/osteoporosis) and diabetes.20
- Conventional DMARDs (disease-modifying antirheumatic drugs), including methotrexate, sulfasalazine, leflunomide, and hydroxychloroquine, may be used singularly or in combination, and are administered orally. These drugs remain the cornerstone of RA therapy but are most effective when introduced early following diagnosis. They reduce pain and inflammation preventing joint damage and preserving joint function.21
The discovery of the role of cytokines in inflammation and the immune response has revolutionised the treatment of RA. A natural substance, cytokines are cells that play a key role in cell growth and the immune response. An increase in cytokines can result in conditions ranging from autoimmune disorders to malignancies. The introduction of biologic agents that can be targeted at specific cells has resulted in vastly improved treatment outcomes.
- bDMARDs (biological disease-modifying antirheumatic drugs) are biologic agents that block cytokine signalling. They are administered by injection and target specific areas of the immune system to reduce inflammation. Initially used in the 1990s, they have proven to be very effective in cases of severe or poorly controlled RA and where conventional DMARD therapy has failed.22
- Janus kinase inhibitors (Jakinib (JAK) inhibitors) are a newer class of bDMARD that work in a different way to earlier bDMARDS, working inside cells. Cytokines rely on the JAK enzymes JAK1, JAK2, JAK3 and tyrosine kinase 2 for signal transmission. JAK inhibitors work “inside” cells, disrupting the cell signalling process that leads to inflammation and the immune response.23 Tofacitinib, a Jak inhibitor administered orally, was noted to result in a 20% improvement in symptoms in some patients (using the criteria of the American College of Rheumatology) but less evidence is available about its efficiency in preventing the progression of the disease in the long term.24 Noted side effects include elevation of blood lipids, impaired liver function tests, myelosuppression, and herpes zoster.25
- Tumour necrosis factor (TNF) inhibitors (or anti-TNF agents, e.g. Etanercept) are a recent development targeting the factor that reduces inflammation and limits further joint damage. Side effects range from minor irritations – such as itchy skin, headaches, and GIT discomfort – to less common but more serious conditions – such as irritation of the optic nerve causing disturbed vision and drug-induced lupus. It is unknown at this stage whether there is a cancer risk with long-term therapy.26
- Surgery may be considered where disease progression has been controlled and pain is associated with existing joint damage rather than ongoing inflammation. As with RA treatment in general, pain relief is the aim of replacing damaged joints.27
Successful treatment outcomes in RA are dependent upon early pharmacological intervention on a “treat-to-target” basis. Choice of therapy is specifically tailored based on individual circumstances, including the severity of the disease, the patient’s response to prior treatment, and any co-morbidities. Effective treatment of RA usually requires the use of several types of therapeutic interventions.28
Future Directions in the Treatment of RA
Mavrilimumab is a granulocyte-macrophage colony-stimulating factor antagonist targeting amino soluble c amino acid soluble cytokine, secreted by a variety of cells. Research to date indicates that it is effective in controlling inflammation and joint erosion in patients with mild to moderate disease who are unresponsive to conventional biological drugs.29
A vaccine-like approach developed by researchers at the University of Queensland (Australia) targets the underlying cause of RA rather than symptoms in patients with CCP-positive arthritis. Nano-technology enables modifying the patient’s lymphocytes not to react to the CCP-antigen, thereby “switching off” the pathological inflammatory response. Trial results to date show this treatment to be both safe and effective with inflammation being significantly reduced. Research is continuing to develop a vaccine that will be readily available on a cost-effective basis.30
Nerve Stimulation Therapy entails stimulation of the vagus nerve in order to “turn off” the inflammatory process. Research into vagus nerve stimulation therapy as an alternative treatment for RA is still in its early stages. Trials are expected to begin in 2018.31
Underwriting RA
Advances in therapy regimes with improved outcomes have enabled insurers to improve the terms on which cover may be provided to sufferers of RA. Applicants diagnosed with RA, either with or without extra-articular manifestations, are in most instances able to obtain Life insurance, generally with some level of extra premium. Where the disease is limited to the joints, Trauma (Critical Illness) benefits are also available with an appropriate premium adjustment and where only very severe forms of Rheumatoid Arthritis are covered.
The progressive nature of the disease, combined with acute on chronic symptomology, need for multiple therapies, and their potential side effects, presents a high risk of disability. However, ongoing developments in therapy with improved patient outcomes may allow disability cover to be made available to RA sufferers in the future.



