-
Property & Casualty
Property & Casualty Overview

Property & Casualty
We offer a full range of reinsurance products and the expertise of our talented reinsurance team.
Expertise
Publication
Use of Artificial Intelligence in Fire Protection and Property Insurance – Opportunities and Challenges
Publication
Public Administrations’ Liability – Jurisprudential Evolution, Insurance Implications, and a Comparative Analysis Across Countries
Publication
Generative Artificial Intelligence and Its Implications for Weather and Climate Risk Management in Insurance
Publication
Engineered Stone – A Real Emergence of Silicosis
Publication
Risk Management Review 2025 -
Life & Health
Life & Health Overview

Life & Health
Gen Re’s valuable insights and risk transfer solutions help clients improve their business results. With tailor-made reinsurance programs, clients can achieve their life & health risk management objectives.
UnderwritingTraining & Education
Publication
Diabetes and Critical Illness Insurance – Bridging the Protection Gap
Publication
Underwriting the Dead? How Smartphones Will Change Outcomes After Sudden Cardiac Arrest
Publication
Always On: Understanding New Age Addictions and Their Implications for Disability Insurance
Publication
Dying Gracefully – Legal, Ethical, and Insurance Perspectives on Medical Assistance in Dying
Publication
AI Agent Potential – How Orchestration and Contextual Foundations Can Reshape (Re)Insurance Workflows Business School
Business School -
Knowledge Center
Knowledge Center Overview

Knowledge Center
Our global experts share their insights on insurance industry topics.
Trending Topics -
About Us
About Us OverviewCorporate Information

Meet Gen Re
Gen Re delivers reinsurance solutions to the Life & Health and Property & Casualty insurance industries.
- Careers Careers
Workers Who Risk Their Skin

August 10, 2015
Ross Campbell
English
If the term “occupational skin disease” conjures images of blackened mediaeval life or besmutted workers toiling at industrial revolution-era machines, then think again. There are over 3,000 known diseases of the skin and many are just as contemporary as the people who suffer with them.1 Medical skin conditions are among the most common of health problems. In the UK, for example, the prevalence of skin diseases in the general population is estimated at 55 %.2 In Germany 23,596 out of a total of 71,263 reported occupational diseases in 2010 were classified as occupational skin diseases. In the US the associated costs of treatment and lost productivity runs to tens of billions of dollars each year.3 In the EU-25 countries, skin diseases rank second in importance to musculoskeletal disorders in occupational disability.4
Only some skin diseases are life threatening – Melanoma is the obvious example – but the impact of all skin diseases is felt psychologically, socially and financially with effects that extend beyond the patients themselves to their families and carers. In a small number of cases, skin complaints are associated with attempted or completed suicide.5 Employment prospects and performance can be blighted by negative feelings toward skin problems and repeated, extended time off for treatment. Disfiguring, irritating skin disease can cause significant interpersonal difficulty, resulting in fragile home and work relationships.6
While the types and frequency of skin disease varies internationally, chronic conditions, such as dermatitis and psoriasis, affect the quality of life of all who experience them. Some skin problems develop from purely medical causes whilst the rest are triggered, and often exacerbated, by individuals’ working conditions. The two factors may co-exist in some individuals. The extent of occupation-related skin disease varies by industry sector but almost always results from an imbalance between the working environment and the natural defence mechanisms of the skin.
Skin deep
Human skin is relatively thin, apart from on the palms of the hands and soles of the feet, yet it provides a protective barrier to light, cold, heat, liquids and micro-organisms. The defence that healthy skin can offer is compromised when its structure is weakened. External contact with certain materials can produce local effects but harmful or toxic agents that breach one or more levels of the skin may cause systemic effects. Understanding why requires a basic knowledge of how skin is constituted.
The outer layers – the epidermis – are predominantly keratin and form a more solid barrier over the more delicate layers below. The topmost epidermis is designed to wear away progressively while the basal layer continually produces new skin cells. The epidermis contains the nerve endings responsible for sensations of pain and its basal layer contains the lymphocytes that provide the immune system response. The elastic collagens in the inner layer – the dermis – are flexible in healthy skin. The dermis is where the blood vessels and sebaceous glands are located. Below this, the hypodermis contains the hair follicles, sweat glands and the capillary network.
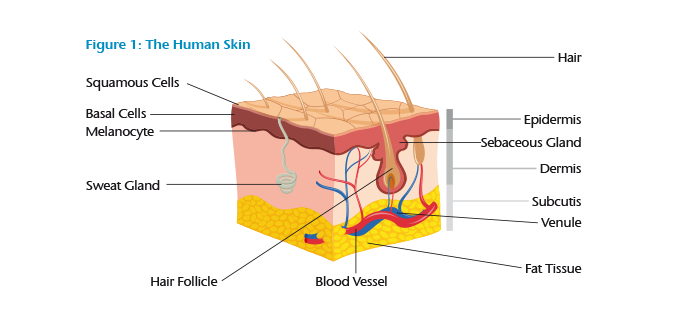
The keratin in the epidermis is resistant to water, water-soluble materials and mild acids. Keratin provides increased protection where it thickens or hardens from exposure to ultra-violet light or friction. The cellular structure of keratin can become swamped by prolonged contact with liquids, causing it to soften. In contrast, if it gets too dry, from exposure to low temperatures or dehydrating agents with high levels of acid or alkali from example, it cracks open and peels apart. These effects both compromise the defence keratin can offer the body from the ingress of harmful materials from outside. Absorption through the skin is further enhanced when it has been altered by physical or chemical injury or by mechanical abrasion of the keratin layer.
Skin disease
The most significant causes of work-related morbidity are dermatitis and psoriasis. Dermatitis (eczema) is acute, or chronic, skin inflammation. Contact dermatitis accounts for at least 80 % of all cases of occupational skin disease. Dermatitis causes widespread inflammation leading to blisters, scaling, peeling, redness, swelling and often extreme itching. In some people, dermatitis is complicated by respiratory conditions: asthma, allergic rhinitis and hay fever. Prolonged sleep deprivation due to nighttime discomfort can result in poor performance at work.
In general dermatitis should not cause disability lasting beyond two weeks; most work-induced dermatitis improves on cessation of contact and with treatment. However it can recur, worsen and spread if working conditions remain unchanged and preventative measures are not implemented. Repeated exposure to irritants and poor care causes the skin to undergo ulcerative change. It cracks and weeps while nails develop chronic dystrophy. Some people develop folliculitis, acne and drug-resistant chloracne – an acne variant indicative of systemic poisoning by certain hydrocarbons. Once chronic, dermatitis becomes much less responsive to treatment even if the causal agents are eliminated.
Psoriasis is a chronic immune condition characterised by accelerated skin cell replacement. Plaque psoriasis, the most common form, causes red, flaky, crusted patches covered with silvery-white scales. Some psoriasis develops into arthritis that limits movement and causes pain and fatigue due to swelling in the joints and connective tissue. Psoriasis can be complicated by exposure to factors encountered at work. The visible disfigurement that results from the illness can cause extreme loss of confidence due to feelings of shame or stigmatization interfering with day-to-day life, the ability to work and may even result in social withdrawal.7
Psoriatic flare-ups usually cause up to two weeks of disability, but more severe manifestations can last much longer. Around 25 % to 30 % of people with psoriasis have it in a moderate to severe form.8 Arthritic involvement worsens the morbidity outlook. In one study, 60 % of participants said psoriasis in the preceding year caused them to take time off work and 40 % reported having not worked owing to it.9 It is also possible that psoriasis predisposes people to poorer health in the long term – sufferers are at elevated risk of developing metabolic and cardiovascular disorders and increased levels of alcohol intake and smoking.10, 11, 12
Environmental causes
Workers who have repeated exposure to sunlight are at risk of developing solar keratosis, severe actinic damage with the chance it becomes squamous cell carcinoma. Artificial ultraviolet (UV) light wavelengths – experienced by workers involved in welding, working with molten metal or glass-blowing for example – can be damaging. The corrosive agents within some dyes and chemicals are activated by certain UV wavelengths. Exposure to radiation from laser light and high-energy sources such as X-rays, radium and other radioactive substances can injure the skin. Prolonged subjection to intensely cold water and very low air temperatures may cause erythema, blistering, ulceration and even gangrene. Waterlogged skin is subject to maceration that can allow bacterial and fungal infection, particularly in overweight and diabetic individuals. In the dry cold, outdoor workers risk frostbite of their fingers, toes, nose and ears.
Conversely, work in an environment with routinely high temperature and humidity levels can induce excess sweating leading to uncomfortable prickly heat, severe chafing and eventually sweat retention syndrome where the ducts become blocked and the epidermis becomes saturated with sweat. Ironically, the heavy protective body wear, boots and gloves that are designed to offer workers protection can worsen these effects.
Some workers' skin is at risk of thermal burns from handling super-heated liquids, such as tar, or operating furnaces or other burning equipment. Construction workers – bricklayers, carpenters, concreters – may handle hazardous materials in the form of oils, preservatives and glues but put their skin at further risk of damage from the vibration of hand tools. Cleaning workers and people working in hotels, restaurants and catering – bakers, butchers, cooks – who do wet-work with soap or detergent, clean silverware, handle acidic fruit juices, animal and vegetable proteins and seafood products are all at risk of irritation dermatitis.
Biological causes
Occupational exposure to bacteria, fungi, viruses or parasites from contact with contaminated material, animals and people puts workers at risk of primary or secondary infections of the skin. Bacterial infections are common in child care settings and in workers who handle animals or animal by-products. Staphylococci and streptococci infections cause boils, carbuncles, pustules and areas of inflammation. Although these have been routinely treated using antibiotics, the increasing fear of antimicrobial resistance, combined with a reduced willingness of doctors to prescribe these treatments, may mean that these once simple conditions are in future associated with disabling illness.
Skin inflammation can result when workers handle certain plants, flowers or wood extracts. Fungal skin infection is common in people exposed to yeasts in bakeries and kitchens. Kitchen staff, cooks, dishwashers and people working to process food often do so in premises with high levels of humidity and temperature during prolonged shifts increasing their risk of developing allergic skin reactions. Humans and animals act as vectors for parasites and workers exposed to either are at risk. Agricultural workers, grain and livestock handlers are exposed to the risk of parasitic infection – scabies and ringworm – as are health care and day care workers. Viral infection, especially herpes zoster, can be unremitting and cause significant discomfort.
Healthcare workers, veterinarians, doctors, dentists and their assistants are at risk from bacterial, viral and mycotic infection from contact with infected blood, saliva and other bodily fluids. They suffer sensitization of the hands from over-washing and develop allergic contact dermatitis from wearing latex gloves. Animal handlers, florists, foresters, gardeners, wine producers and fruit growers are at similar risk from exposure to mycotic and microbial agents and from parasitosis through contact with fungi, yeasts, bacilli and animal parasites.
Mechanical causes
Mechanical trauma of the skin may be mild or moderate in degree. Injuries such as cuts and blisters can be sustained from using hand tools. These abrasions can allow secondary bacterial or fungal infection. Trauma may induce chronic changes in the skin as a result of scar, callus or keloid formation. Scratching or an isomorphic reaction to the trauma site by people who have skin disease such as psoriasis may exacerbate this.
Workers who use pneumatic tools – riveters, drills or hammers – are at risk of soft tissue and fibrous damage from repetitive trauma. The prolonged use of power tools, or indeed any machine developing intense levels of vibration, induce painful spasms in the fingers and hands or cause long-term peripheral vascular damage. Losing control of machinery can lead to shearing of tissue, laceration and deep skin abrasion.
Mechanical factors that lead to skin damage include repeated friction and excessive or prolonged pressure. Often both occur together. Friction, pressure and trauma may induce changes ranging from callus and blisters to myositis, tenosynovitis, bony injury, nerve damage or laceration. Friction may result from handling abrasive materials, or using some industrial dusts, whose effects are a function of the shape and size of the dust particles and the extent of their friction with the skin.
Chemical causes
Most occupational dermatitis is the result of contact with chemicals. The effects vary from simple drying of the skin to painful inflammation and even total cell necrosis. Organic and inorganic chemicals are common irritants that are responsible for purely allergic or photo-sensitive reactions that may even lead to permanent skin decolouration.
Chemicals that injure the skin are either “allergic sensitizers” – compounds that with repeated exposure cause hypersensitivity and adverse reactions – or they are “primary skin irritants”. Primary irritants are concentrated acids and alkalis, metallic salts and certain gases and solvents that can cause near-instant skin damage. Repeated exposure to these so-called primary irritants in more dilute concentrations, in milder solvents or water-soluble fluids, is needed before the effects are felt.
Some of the toxic chemicals used in industry and agriculture cause direct harm to the skin surface. Contact with solvents, mineral fibres, detergents, biocides and pesticides can produce local effects such as irritation, intense urticaria and pruritus, even ulceration and burning.
Workers are also vulnerable to systemic intoxication if harmful substances are absorbed through the keratin and epidermal cell layers and transferred into the blood stream or lymphatic system. They can be transported to vulnerable target organs with grave health consequences. Mishandling of chemicals, perhaps by circumventing safe practices, or by misuse, such as cleaning oiled hands with benzene, can play a role in cutaneous absorption.
Hairdressers, beauticians and manicurists suffer dermatitis from handling the ammonia, bleach and solvents in treatment and beauty products. Metal and electro-mechanical engineers – machinists, mechanics, platers and electronics workers – develop dermatitis from handling glues, oils and grease, chemical cleaning products and following the abrasive damage caused by metallic particles and acids. Painters, sprayers and decorators handle varnishes, resins, pigments and thinners that contain harmful chemicals injurious to the skin.
Conclusion
Occupational skin disease can result from an environmental, biological, mechanical and chemical cause or a combination of these factors. In addition, some people have a pre-disposition to developing problems – perhaps the result of having delicate skin or a low tolerance to certain working conditions or materials to which their work exposes them. Other people find a pre-existing skin condition is made worse by particular work tasks, exposure to hazardous material or from wearing heavy protective gear.
The effects on the skin may range from very slight erythema (reddening) or permanent discoloration of the skin to far more complex changes, even including malignancy. Disability hinges of the severity of the skin condition and the demands of the occupation. Care is needed when assessing claimants with jobs that demand good skin condition or whose working environment is likely to cause them further problems.



