-
Property & Casualty
Property & Casualty Overview

Property & Casualty
We offer a full range of reinsurance products and the expertise of our talented reinsurance team.
Trending Topics
Publication
Engineered Stone – A Real Emergence of Silicosis
Publication
Use of Artificial Intelligence in Fire Protection and Property Insurance – Opportunities and Challenges
Publication
Generative Artificial Intelligence and Its Implications for Weather and Climate Risk Management in Insurance
Publication
Public Administrations’ Liability – Jurisprudential Evolution, Insurance Implications, and a Comparative Analysis Across Countries
Publication
Risk Management Review 2025
Publication
Who’s Really Behind That Lawsuit? – Claims Handling Challenges From Third-Party Litigation Funding -
Life & Health
Life & Health Overview

Life & Health
We offer a full range of reinsurance products and the expertise of our talented reinsurance team.
Training & Education
Publication
AI Agent Potential – How Orchestration and Contextual Foundations Can Reshape (Re)Insurance Workflows
Publication
Diabetes and Critical Illness Insurance – Bridging the Protection Gap
Publication
Group Medical EOI Underwriting – Snapshot of U.S. Benchmark Survey
Publication
Why HIV Progress Matters
Publication
Dying Gracefully – Legal, Ethical, and Insurance Perspectives on Medical Assistance in Dying Moving The Dial On Mental Health
Moving The Dial On Mental Health -
Knowledge Center
Knowledge Center Overview

Knowledge Center
Our global experts share their insights on insurance industry topics.
Trending Topics -
About Us
About Us OverviewCorporate Information

Meet Gen Re
Gen Re delivers reinsurance solutions to the Life & Health and Property & Casualty insurance industries.
- Careers Careers
Listeriosis – One of the Notifiable Diseases

April 30, 2018
Alice Coyne, Zakira Parker
Region: South Africa
English
Listeriosis is a bacterial infection caused by the gram-positive motile bacterium, Listeria monocytogenes.1 The organism is an environmental pathogen widely distributed in nature and can be found in soil, water, sewage and decaying vegetables. Animals and food products can become contaminated from these sources at any time. As a result, anyone can get Listeriosis. Those at high risk of severe disease are newborns, the elderly, immunocompromised individuals, pregnant women and their unborn babies. There is no transfer of Listeriosis from human to human, but it can be transferred from a pregnant woman to her fetus or nursing baby.
Signs and Symptoms
In healthy adults, symptoms are usually mild and may include fever, and sometimes nausea and diarrhoea. Symptoms in those with invasive Listeriosis, where the bacteria have spread beyond the gut, include febrile gastroenteritis, sepsis, or meningitis.2 Those with invasive listeriosis usually report symptoms starting one to four weeks after eating contaminated foods; some people have reported symptoms starting as late as 70 days after exposure or as early as the same day of exposure.3 Healthy adults with a strong immune system might not experience any signs or symptoms; instead, they act as a carrier for the bacteria.
Pregnant women typically experience only fever and other flu-like symptoms, such as fatigue and muscle aches. However, infections during pregnancy can lead to miscarriage, stillbirth, premature delivery, or life-threatening infection to the newborn. People other than pregnant women, may experience symptoms that include headache, stiff neck, confusion, loss of balance and convulsions, in addition to fever and muscle aches.
Causes
Listeriosis is usually spread through the ingestion of contaminated food products, most frequently fresh and frozen poultry, processed meats, raw or unpasteurised milk, cheeses, fresh produce including fruit and vegetables, and smoked fish products. Its optimum growth temperature is between 30°C and 37°C. Unlike most food pathogens, Listeria can continue growing in food stored the fridge and can survive in temperatures of 4°C.4 The infection incubates for between three and seventy days and up to 10% of people may be asymptomatic carriers. Outbreaks of Listeria in food are common across the world. These outbreaks present the same problem: the source of contaminated food is difficult to identify. The incubation period of 70 days makes it difficult to track what the patient has eaten and therefore to identify the contaminated food.
Diagnosis and Treatment
Listeriosis is usually diagnosed when a bacterial culture grows Listeria Monocytogenes from body tissue or fluid, such as blood, spinal fluid or the placenta. Because few symptoms are unique to Listeriosis, medical practitioners may consider a variety of potential causes for infection, including viral infections – such as flu – and other bacterial infections that may cause sepsis or meningitis.5
Listeria infections typically resolve without treatment, but antibiotics may be necessary to treat some cases. Although there have been no studies done to determine what drugs or treatment duration is best, ampicillin is generally considered the preferred agent.6
Prevention
Unlike most other foodborne pathogens, Listeria can grow in refrigerated foods that are contaminated. To prevent this, it is recommended to have fridge temperatures below 4°C, and freezer temperatures below -18°C.7
People at high risk should avoid raw/unpasteurized milk and milk products. Thoroughly cook animal foods, such as meat, poultry or fish – overcook rather than undercook – and keep an eye on the expiry dates of perishable foods.
There is no vaccine or pre-exposure prophylaxis for preventing infection. The main preventive measure is to always ensure that good basic hygiene is followed. This includes knowing the risks of food poisoning and following the Clean, Separate, Cook and Chill guidelines, recommended by the Centres for Disease Control and Prevention (CDC) in the U.S.8
The CDC also recommends a few basic steps to prevent infection with Listeria (and other foodborne diseases):
- Wash and handle food properly.
- Keep a clean kitchen/eating environment.
- Thoroughly cook meat and poultry.
- Store foods properly – consume ready-to-eat foods as soon as you can, and never store in the refrigerator beyond the use by date.
- Eat safer foods.
Given its widespread presence in the environment, and the fact that the vast majority of Listeria infections are the result of consuming contaminated food, preventing illness is necessarily and understandably a food safety issue.
Epidemiology
General Incidence
In South Africa, the National Institute for Communicable Diseases has added Listeriosis to its list of notifiable diseases. According to the World Health Origination, the current outbreak of Listeriosis in South Africa is the largest in recorded history.9 So far 767 cases have been confirmed, of which 81 people have passed away.10 The first documented outbreak of Listeriosis in South Africa was in 1977, where from August 1977 to April 1978, 14 cases were reported in the Johannesburg area.11
In the U.S., the last big Listeriosis outbreak was in 2011 where 147 cases were recorded and 30 people died from the disease.12 From 1998 to 2016, the U.S. had a total of 68 outbreaks, resulting in 132 deaths from 860 illnesses.13
In Europe Listeriosis has a fairly low prevalence of approximately five cases per million of the population each year, although this rate does differ from one country to the next.14
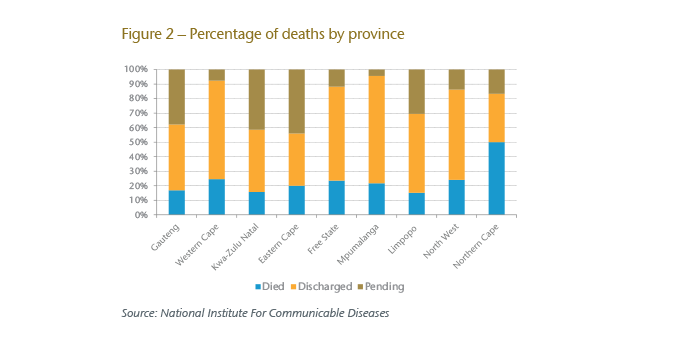
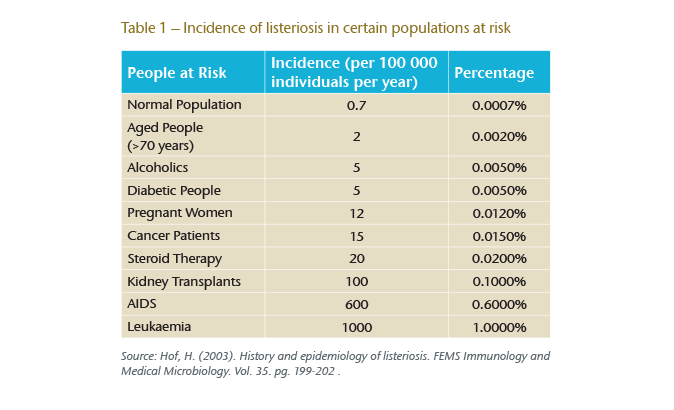
Listeriosis has a relatively high mortality rate, between 20% and 25%, compared to other foodborne pathogens – such as Salmonella or E. Coli – that have an overall mortality rate of 1%, and a 5% mortality for individuals with a health immune system.15
Pregnant women make up about 30% of all reported cases, and in approximately 49% of cases, the person had a compromised immune system.16
Current outbreak stats in South Africa
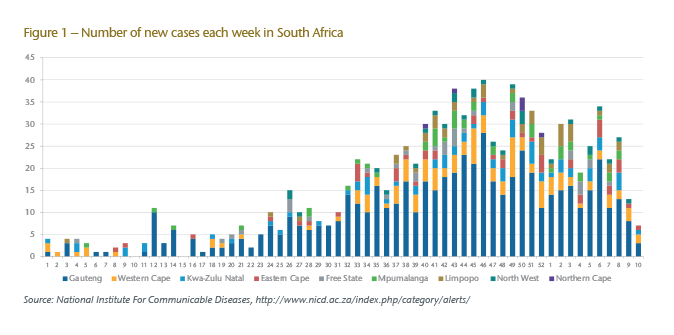
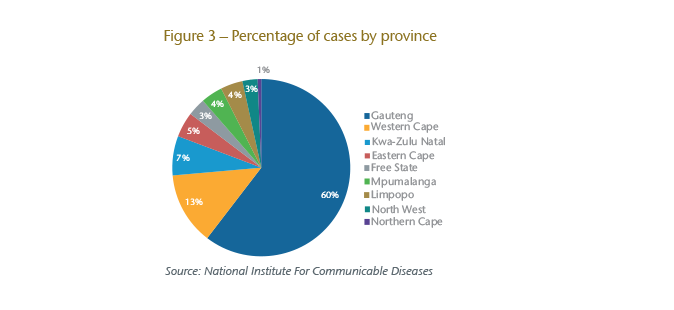
Cases of Listeriosis have been reported across all nine provinces in South Africa. The majority of the cases come from Gauteng, with a total of 462 cases reported.17 The Western Cape has the second highest prevalence of the disease with a total of 101 cases, followed by Kwa-Zulu Natal with 55 cases reported.18
In Gauteng the population incidence rates have increased from two per million to eight per million.19 The highest incidence has been recorded in the City of Johannesburg at 12 cases per million.20
Pregnant women are about 20 times more likely to get Listeriosis than normal adults with a healthy immune system.21 Approximately 40% of the reported cases have been neonates.22 Listeriosis commonly affects people with weak immune systems such as those with cancer, HIV, or diabetes. From the adults whose HIV status was known, 78% of those who had Listeriosis were HIV positive.23
In early March 2018, the source of Listeriosis was thought to be found. Serveral factories have since be closed down, and their meat product has been recalled. Unfortunately, this has only been linked to one source of Listeriosis, so the outbreak is still continuing.
Conclusion
While high levels of public awareness have been generated, understanding the mortality threat from infection by this organism will assist underwriters in identifying lives that are more at risk. Applicants with existing morbidity, and who are at increased mortality risk if infected, will continue to be identified. However, minor symptoms, often explicitly including influenza, are outside the scope of required disclosure for life and health products. The variable incubation period and uncertainty over diagnosis means that it is unlikely that applicants who have Listeriosis will be recognised at underwriting stage.
Given the current volumes, it is not expected that Listeriosis will have a large impact on individual life claims as most underwritten lives have healthy immune systems. We may see a few additional claims on short-term sickness products or income benefits with a short waiting period. These claims will be managed as any other short-term sickness claim. On group business where we see a relatively high proportion of HIV positive lives, there may be slightly increased mortality.




