-
Property & Casualty
Property & Casualty Overview

Property & Casualty
We offer a full range of reinsurance products and the expertise of our talented reinsurance team.
Trending Topics
Publication
Engineered Stone – A Real Emergence of Silicosis
Publication
Use of Artificial Intelligence in Fire Protection and Property Insurance – Opportunities and Challenges
Publication
Generative Artificial Intelligence and Its Implications for Weather and Climate Risk Management in Insurance
Publication
Public Administrations’ Liability – Jurisprudential Evolution, Insurance Implications, and a Comparative Analysis Across Countries
Publication
Risk Management Review 2025
Publication
Who’s Really Behind That Lawsuit? – Claims Handling Challenges From Third-Party Litigation Funding -
Life & Health
Life & Health Overview

Life & Health
We offer a full range of reinsurance products and the expertise of our talented reinsurance team.
Training & Education
Publication
AI Agent Potential – How Orchestration and Contextual Foundations Can Reshape (Re)Insurance Workflows
Publication
Diabetes and Critical Illness Insurance – Bridging the Protection Gap
Publication
Group Medical EOI Underwriting – Snapshot of U.S. Benchmark Survey
Publication
Why HIV Progress Matters
Publication
Dying Gracefully – Legal, Ethical, and Insurance Perspectives on Medical Assistance in Dying Moving The Dial On Mental Health
Moving The Dial On Mental Health -
Knowledge Center
Knowledge Center Overview

Knowledge Center
Our global experts share their insights on insurance industry topics.
Trending Topics -
About Us
About Us OverviewCorporate Information

Meet Gen Re
Gen Re delivers reinsurance solutions to the Life & Health and Property & Casualty insurance industries.
- Careers Careers
The Rise and Rise of Childhood Mental Disorders: Overdiagnosis or Epidemic?

August 25, 2015
Dr. Chris Ball,
Lynn Baillie, Senior Underwriting Expert, London
English
Diagnostic fashions are of keen interest to life and health insurance practitioners because they challenge current and traditional underwriting practice. The methodical processes by which risk selection guidelines are updated make speedy reaction to abrupt changes in diagnostics or medical practice problematic.
This is especially acute where many more diagnoses are made in children, the long-term consequences of which cannot be known, or in adults when the problems have clearly been present since their early years. Nowhere is this more clearly illustrated than by the increase in the diagnosis of children experiencing a mental disorder.
The conditions that are of highest profile are autistic spectrum disorders (ASDs) and attention deficit hyperactivity disorder (ADHD), but childhood bipolar disorder has also received much attention.2 Diagnoses of both have increased significantly over the past decade prompting some commentators to voice concern about the impact of labelling, stigma and overdiagnosis. Others have suggested we are in the midst of a preventable epidemic that will have long-term consequences unless the issues are addressed.3 The situation is further complicated as 41 – 95 % of those with a primary diagnosis of ADHD also exhibit autistic traits, and of those with a primary diagnosis of ASD between 18 – 30 % also meet the criteria for ADHD.4,5,6 This article explores the implications of ASD and ADHD for the insurance industry.
Clinical syndromes of ASD
The ASD range includes autism itself, Asperger’s syndrome and childhood disintegrative disorder amongst other rarer forms. The DSM-5 combines them in a single category with “specifiers” for the severity depending on the support needed day to day.7 Symptoms are usually evident by the time a child is three years old but often the diagnosis is made much later. The condition is life-long.
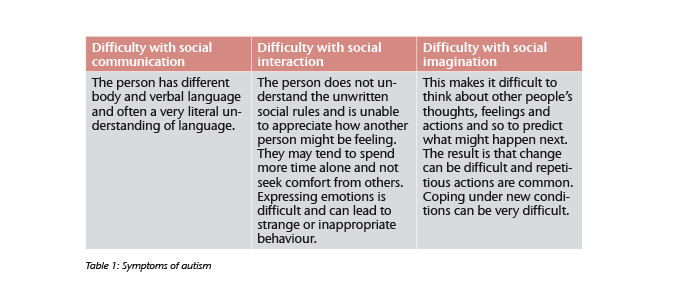
The core symptoms are usually grouped under three categories – social interaction, social communication and social imagination (see table 1) – although DSM-5 has conflated them into social communication and interaction alone. In addition to these problems there are often concurrent difficulties such as intellectual disability, other mental health problems and physical disorders.
Comorbid conditions are common with epilepsy being a major issue – particularly complex partial seizures. Sleep disorders and gastrointestinal problems are associated with behavioural disturbance and poorer outcome. It can be very difficult to diagnose any medical or mental health problem in this group of people as many are only able to communicate their distress through behavioural disturbance and find it difficult to cooperate with examinations and investigations. As a result, diagnoses can be made later than they otherwise might be.8
Systematic long-term outcome studies of those who experience ASDs are rare. Sample sizes are often small, follow-up periods not long and they are restricted to relatively young ages.9,10,11,12 Pulling these disparate studies together, Woolfenden et al. (2012) suggested that a standardised mortality ratio (SMR) of 2.6 was realistic.13 What this hides is an enormous variation depending upon the clinical picture. A consistent finding is that females have a lower SMR than males (e. g. 2.1 vs 7.2).14 This may be a reflection of the relative levels of intellectual disability (IQ) between the sexes, as those with the greatest degree of intellectual disability have a greater SMR. The association is strengthened by the observation that where the person has a low IQ they are more likely to have epilepsy. Also, mortality is raised in those who have epilepsy.15 Mouriden (2013) also draws attention to the high number of accidental deaths, particularly by suffocation and drowning, most prevalent in the more severely impaired group.16 Once again there may be some overlap with epilepsy.
Autistic spectrum disorders – Rising numbers?
A dramatic rise in ASDs has been reported in the U. S. where The Centres for Disease Control and Prevention identified a 78 % increase between 2002 and 2008.17 While the UK experienced increased diagnosis rates in the 1990s, a more recent study revealed stable yearly prevalence rates; 3.8 per 1000 boys and 0.8 per 1000 girls.18 The National Autistic Society (NAS) has highlighted the impact of growing older with ASD and, more particularly, the effect it has on people who only receive their diagnosis late in life. In an NAS survey, 71 % of respondents over age 55 had been diagnosed during the previous ten years.19
ASD was once thought to be rare – around 1 in 2000 people being affected – but there are good reasons why growing numbers are now labelled with ASD. Announcements such as that from singer Susan Boyle that she has Asperger’s syndrome may do more to highlight the issue than any number of more formal initiatives.20 General awareness of the problem has grown as more people are identified through medical services and this in turn prompted an increase in population-based studies. But studies raise a dilemma; do the new numbers represent a “true increase” in prevalence or have changing diagnostic criteria simply driven them up?21 Longitudinal population-based studies using consistent diagnostic criteria can demonstrate if change is real but they are expensive and impractical.
When DSM-IV22 and ICD-1023 criteria are used to identify the wider spectrum ASD up to 7 per 1000 are identified, ten times more than using earlier criteria. More recent studies place the level at over 2 % in some areas of Europe, Asia and North America. This makes it clear that the criterion used to identify ASD has a significant impact on the prevalence figures.24 In England the Adult Household Psychiatric Survey (2009) used a screening tool, the autism quotient, to identify those who then went on to structured interviews designed to identify ASD. The prevalence of the disorder was 1.8 % of men and 0.2 % of women. This sex ratio is a common finding.25
Clinical syndromes in adult attention deficit hyperactivity disorder (ADHD)
In children, a diagnosis of ADHD is made as much on the report of parents and teachers as on examination of the child. In adulthood much more reliance is put on the patients’ report but histories from partners and parents are still valuable. Recollection of childhood is notoriously unreliable with an underreporting of problems by the patient when compared to other informants.26 The earlier definitions of ADHD made little reference to the developmental stage of the patient and as a result many received a diagnosis of “ADHD in partial remission” despite the problems experienced.27
The DSM-IV laid down the basis for current diagnostic practice with two distinct symptom patterns identified: Inattentive type and hyperactive-impulsive type. Both sets of symptoms are combined in some individuals.28 DSM-5 broadly follows this line but asks for fewer symptoms when making the diagnosis in an adult and broadens the age of onset to 12.29 ICD-10 has generally similar criteria but tends to be rather stricter than either DSM criteria.30
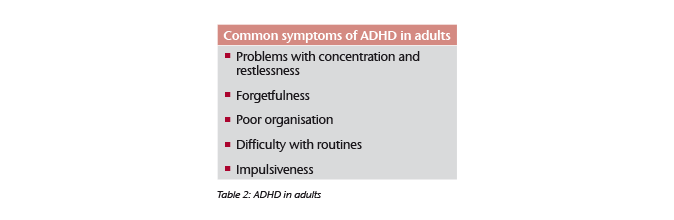
Impulsiveness
Many patients will also experience swings in their mood with frequent highs and lows. Most people at the age 30 have entered a more stable phase of their lives, but those with ADHD will often have short-lived jobs and relationships, failing to reach their full potential. They are more likely to have accidents and live in an unhealthy manner. There is an association with anti-social personality disorder which can lead to problems with the law.31 Difficulties with attention mean that completing courses of study is hard and so there is a record of underachievement, academically and in the workplace. Sufferers from adult ADHD frequently have other mental health problems, from anxiety and depression to sleep disorders, autism and substance misuse.32
The rise in numbers of young people on prescribed medication is a cause of significant concern in some quarters.33 Stimulants (e. g. methylphenidate) are the mainstay of pharmacological management, being effective in about 70 % of patients.34 Medication has an impact not only on the core symptoms but also on issues such as poor self-esteem, anger outbursts and cognitive problems. For most, the medication is tolerated well but can increase blood pressure and heart rate, raising concerns about future cardiovascular risk. These risks appear small but the longer-term effects are not yet clear.35 Despite obvious worries it does not appear that using methylphenidate per se leads to addiction.36
Because ADHD was regarded as a childhood disorder there are very few long-term outcome studies to guide the insurer. For many it remains a life-long condition whose impact varies with the demands of being a grown-up. Medication is not a cure and symptoms may return if the medication is stopped. The economic burden of the disorder is high with increased sick leave, poor productivity and more accidents contributing to the cost. Adult ADHD has been positively associated with lung disease, cardiovascular problems and a number of other chronic diseases.37 There is a significant association with suicide, depression and other mental health disorders later in life that may influence the prognosis.
Given these multiple problems, it is perhaps not surprising that for those diagnosed in childhood an SMR of 1.88 has been reported after following the participants to a mean age of 30.38 What the longer-term prognosis for this group will be remains to be reported.
Attention deficit hyperactivity disorder (ADHD) – Rising numbers?
ADHD is one of the commonest psychiatric disorders of children and until relatively recently it was believed that the disorder resolved as the person matured. The increases in diagnosis are particularly marked in the U. S. with the New York Times reporting 41 % increase over the last decade.39 The diagnosis is much less likely to be made in the UK. Only 1.5 % of parents in the UK reported a diagnosis for children age 5 – 9 by contrast with 6.3 % in the U. S. This comes about from a more stringent use of the criteria and more concerns about the use of medication.40
Cases of adult ADHD began to be reported in the mid-1970s but rather than being exceptional cases that persist, it has become clear that the condition very frequently continues into adult life. For those diagnosed in childhood, Faraone et al. (2008) conclude that at the age of 25 about 15 % retain enough symptomatology to receive a full diagnosis whilst another 50 % are in “partial remission”.41 Although many symptoms ameliorate as the person grows older the differences with those who are “normal” are maintained because of the maturation that goes with normal ageing. The prevalence of the disorder in adults has been reported in the range of 2 – 5 %. In those who experience mental health problems such as anxiety and depression the rate is much higher, 10 – 20 %. Unsurprisingly, the rates are even higher in those attending forensic or addiction clinics.42
Overdiagnosis or epidemic?
- No overdiagnosis, no epidemic
- Only recognising what was always there
Improved diagnostic criteria are more sensitive and pick up more people who have these disorders.43 With the improvement in treatments, both psychological and pharmaceutical, and the increasing awareness of the neuro-biological underpinnings, there is now a value in making the diagnosis even in minor cases. Associated with this is the need for a diagnosis in order to get access to specialist educational resources.44 - These changes make the public and the clinician more aware of the possible diagnoses, a process also driven by the revolution in information technology.45
- There is now an understanding with ADHD that this is not a disorder that people grow out of but gives life-long problems for many.46
- Only recognising what was always there
- Epidemic
- Change in the environment
The developing brain is particularly sensitive to environmental toxins. With the rise in industrialisation and pollution more people are exposed. The now discredited theory that the NMR vaccine causes ASD is most notorious of these theories but there is no doubt that the dopamine containing neurones of the brain reward systems are particularly sensitive to environmental causes of damage.47 - Changes in genes
Both disorders have a high degree of heritability, with overt genetic abnormalities present in some. It has been argued that this is likely to change in the future with the segregation of people with particular talents into specific industries (e. g. computing), increasing the likelihood that their offspring will suffer more serious forms of the disorder.48 - The way we live now
The disruption of the normal light/dark cycles by television and computers disturbs the normal circadian rhythms of the brain. Much of the geographical variance in diagnosis has been ascribed to solar intensity.49
- Change in the environment
- Overdiagnosis
- General trend to diagnose all human behaviour
Publication of the DSM-5 brought forth a torrent of controversy with the assertion that many more human behaviours could now attract a mental health diagnosis. The diagnostic criteria for both disorders have loosened.50 - We would rather our children be ill than difficult
Living in a perfectionist society it is much better that our children have an illness than are difficult to manage. This changes the dynamic with society, as the response to a sick child is very different to the response to a difficult one. Access to services also drives this process as above.51 - Big pharma
The pharmaceutical companies have a vested interest in developing markets that have not yet been exploited to the full. Some have argued that their promotion of medication in children is a cynical manoeuvre to maximise profits driving the diagnostic process for profit.52
- General trend to diagnose all human behaviour
Implications for insurers
As those who were diagnosed in the 1990s grow older and with an increasing number of people receiving an ASD diagnosis in adulthood insurers are likely to see more applicants with the diagnosis. By and large they are likely to be those with “high functioning” autism or Asperger’s syndrome. Many of this group will have a normal life expectancy as the major risk factors for early mortality, low IQ and epilepsy, are absent. Attention must be paid to comorbidities such as epilepsy, sleep disorders and mental health problems all of which can reduce life expectancy. Insurers can no longer rely on ratings that suggest that ASDs are rare disorders with a significantly reduced life expectancy if they are not to disadvantage a growing group increasingly in need of financial services.
To date insurers will have seen very few applicants in either category and they will have been a self-selecting group who are high functioning. For those with childhood diagnosis of ADHD it is likely that those for whom the problems have receded are applying for cover. This fact is reflected in manuals who suggest this very narrow group can be taken on at standard rates. Clearly care must be taken with those who experience comorbid conditions in their physical or mental health and ratings need to be applied appropriately.
The rise in the numbers of those who are diagnosed with ASDs is not likely to change the situation greatly as the growth is largely in the higher functioning group. The changes in ADHD present a different challenge as less is known about the long-term outcome for this group and the effects of long-term cardiovascular impact of stimulants. The effectiveness of the treatment may also draw people into economic spheres where they need and expect insurance services which would not have been the case in the past.
The approach to disability insurance and income protection (IP) for these groups has been very conservative in the past with many insurers unwilling to offer terms. The rise in diagnoses of those who are high functioning with ASD will probably present relatively little excess risk and those with ADHD who respond well to medication may also function well and consistently over many years. The underwriter needs to be aware of the employment record of these applicants, and where it can be seen to be stable over time terms should be available.
Overdiagnosis or epidemic?
With a degree of inevitability one must conclude that the jury is still out on the issue of epidemic versus overdiagnosis and not likely to return a verdict in the immediate future. The arguments around the growth in diagnosis are summarised in the adjacent panel. Whatever the ultimate conclusion to this debate the insurer has a challenge to meet with these disorders. The traditional stances on underwriting are being challenged as the numbers with milder forms of the disease are being identified and so new philosophies need to be devised to offer this group suitable products at competitive prices.
Understanding the manner in which these developmental disorders affect the course of a person’s life is key to this process accompanied by a realistic assessment of the comorbidities, medical and social, that go along with the diagnoses.





