-
Property & Casualty
Property & Casualty Overview

Property & Casualty
We offer a full range of reinsurance products and the expertise of our talented reinsurance team.
Expertise
Publication
Biometric Information Privacy – Statutes, Claims and Litigation [Update]
Publication
Inflation – What’s Next for the Insurance Industry and the Policyholders it Serves?
Publication
Human Activity Generates Carbon and Warms the Atmosphere. Is Human Ingenuity Part of the Solution?
Publication
Illinois Changes Stance on Construction Defect Claims – The Trend Continues
Publication
Generative Artificial Intelligence in Insurance – Four Aspects of the Current Debate
Publication
Battered Umbrella – A Market in Urgent Need of Fixing -
Life & Health
Life & Health Overview

Life & Health
We offer a full range of reinsurance products and the expertise of our talented reinsurance team.

Publication
Underwriting High Net Worth Foreign Nationals – Considerations for U.S. Life Insurance Companies
Publication
Group Term Life Rate & Risk Management – Results of 2023 U.S. Survey
Publication
Trend Spotting on the Accelerated Underwriting Journey
Publication
All in a Day’s Work – The Impact of Non-Medical Factors in Disability Claims U.S. Industry Events
U.S. Industry Events
Publication
Marginal Gains in the Medicare Supplement Market -
Knowledge Center
Knowledge Center Overview

Knowledge Center
Our global experts share their insights on insurance industry topics.
Trending Topics -
About Us
About Us OverviewCorporate Information

Meet Gen Re
Gen Re delivers reinsurance solutions to the Life & Health and Property & Casualty insurance industries.
- Careers Careers
Understanding Past Mortality Patterns in Germany

April 21, 2020
Beata Puls,
Valeria Walter
Region: Germany
English
Deutsch
Managing mortality risks is at the core of the Life insurance business. This article presents the results of our comprehensive analysis of population mortality trends in Germany. The analysis was carried out before COVID-19 became a global pandemic. No one knows exactly how this disease will affect the development of mortality risk. It is expected that COVID-19 will have some impact on German population mortality in 2020 and 2021. From today’s perspective, however, it can be assumed that in two or three years time the mortality improvements will again be in line with historic mortality trends. Despite COVID-19, these trends remain highly important for Life insurance.
In our comprehensive mortality study, we focused on the middle ages 20–69 that are most relevant for mortality products in Germany.1 Based on mortality data from the Human Mortality Database for West Germany, the 20-year rolling trend revealed improvements in mortality for (almost) all years and ages.
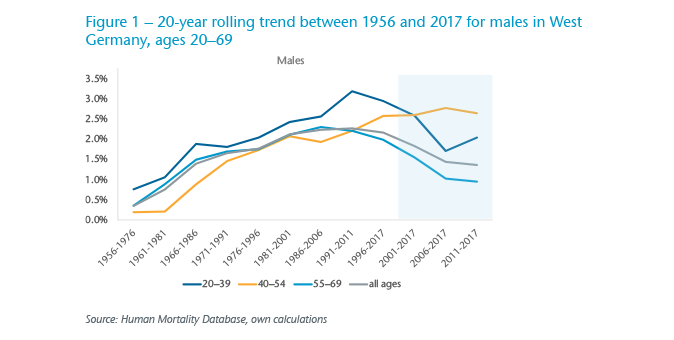
For males, mortality improvements increased for all ages until 2011, with very high gains, especially for young ages. After 2011, there was a slowdown in improvements although mortality trends were still positive; the continued increase in improvements were for middle ages (45–54) only.
The corresponding results for females are more volatile due to the naturally lower number of death cases in women in the considered ages – 65% of all cases are males – but they do show that the slowdown in mortality improvements started slightly earlier than for males. Another difference between the sexes is the very weak improvements for females in high ages.
Adding in information on the causes of death again produced some contrasts across age groups and gender. Not surprisingly perhaps, circulatory system diseases are the main cause of death among elderly people. However, neoplasms are the leading cause of death in the age bracket 20–69, accounting for almost 35% of deaths in males and 50% of deaths in females in 2017.
Meanwhile, external causes are the leading cause of death for young ages (up to 60% in 20–24-year-old males) underlining how the dominant cause of death changes as we move through age bands. Traffic accidents and suicides are notable components in this cohort.
A closer look at the distribution by cause of death and year for ages 20–69 reveals that circulatory system diseases were the leading causes of death until 1991 for males, but were steadily decreasing. For females it was always cancer, which for both genders is gradually increasing over the observation period. Cancer is now the main cause of death in ages for both sexes in Germany, as it is in other high-income countries. One reason could be the big advances that have been made in treating circulatory or cardiovascular conditions. Another explanation for the shrinking share of circulatory system diseases could be the change in the documentation required on death certificates in Germany. New instructions stipulate a less biased medical judgement, which explains the growing share of unspecified causes of death in recent years.
Heat maps and hot spots
Some of the most interesting trends were highlighted by the heat maps we generated using the available data. For example, the heat map for men in Figure 2 shows two hot spots. In 1968/1970 the most likely cause of the deterioration in mortality was the Hong Kong flu that caused about one million deaths worldwide. Whether COVID-19 renders a comparable effect on mortality cannot be predicted at this stage. The hot spot around 1990 can be attributed to deaths from AIDS and an increase in deaths from drug abuse. Today people with HIV don’t necessarily die of the disease, thanks to big advances in available therapies.
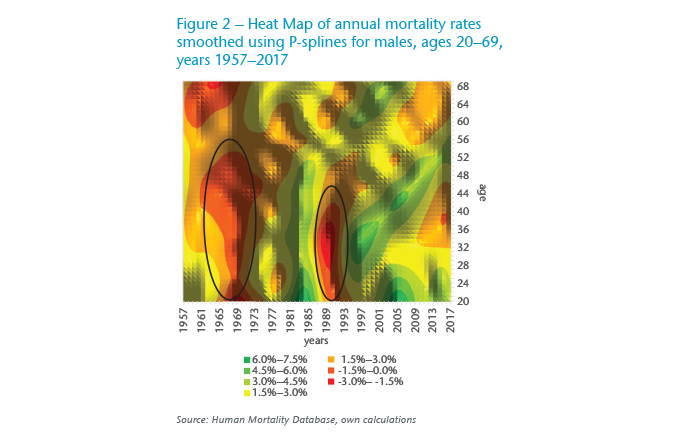
The slowing down of mortality improvements in recent years is clearly visible in the orange coloured areas to the right on this heat map.
The strongest slowdown of improvements came in two age bands: 30–39 and 60–69 (Figure 3). In the former group, the deceleration stemmed from a slowdown in improvements from external causes, which comprise mainly intentional self-harm and accidents, from weaker improvements in neoplasms (especially lymphoid and hematopoietic tissues), diseases of the digestive system (e.g., alcoholic cirrhosis of liver) and mental and behavioural disorders that are mainly linked to drug and alcohol abuse.
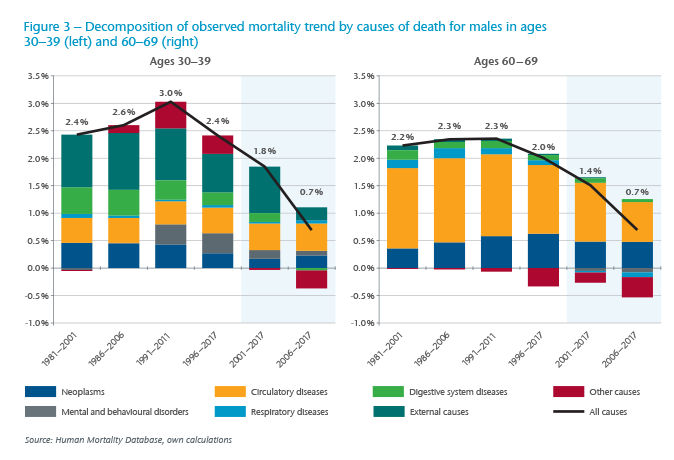
Specifically, the high mortality improvements from suicides and traffic accidents that were observed between the mid-90s and the mid-2000s stagnated in the more recent years.
In the 60–69 age group there was a marked slowdown in improvements from circulatory diseases. Mortality increased due to some other causes of death where a significant contribution of the development is attributable to unspecified causes and also due to respiratory diseases linked to chronic obstructive pulmonary disease.
A common characteristic for both considered age groups was a slowdown of improvements in so-called diseases of despair. Unlike the United States, where the middle ages are most affected by the opioid crisis, drug dependence doesn’t play such a significant role in mortality developments of diseases of despair for men in Germany. One possible reason for the differences between Germany and the U.S. in drug abuse is the effectiveness of the German welfare system and mandatory health insurance. Also, pharmaceutical regulations in Germany may have been more successful than in the U.S. in preventing large-scale drug addiction and its related mortality.
Nevertheless, the insurance industry should continue to monitor the situation in Germany and elsewhere for a potential uptick in opioid addiction.
Female variations
The mortality heat map for females is characterised by the post war cohort effect having a strong negative impact on mortality. The main reasons for this effect are stronger deteriorations due to lung cancer, compared with neighbouring cohorts, and a worsening due to respiratory diseases in high ages; weaker improvements in circulatory system diseases are also in evidence. Respiratory diseases are mainly linked to COPD; the majority of these cases in high-income countries can be attributed to smoking.
We assume that although the 1941–1950 birth cohort does not have the highest smoking prevalence, women of this cohort smoke for longer than the later cohorts with higher peaks.
As cancer has increasingly gained in importance throughout the years, it is of particular interest to look into the decomposition of cancer sites where slowdowns or even deterioration in overall mortality trends were observed in recent years. The breakdown for younger and older females presents a somewhat mixed picture. In the 60–69 age band, lung cancer has the biggest negative contribution with strong deterioration in recent years; in breast cancer, however, strong improvements partly mitigate this effect.
Conversely, in the 25–45 age band lung cancer has a small impact on cancer mortality. However, there were smaller improvements or even deterioration in cancer mortality from breast cancer in recent years.
The big picture
Looking at the heat maps for males and females together, we can see a positive trend in mortality for (almost) all years and ages after 1980. The improvement was particularly strong for the male cohort born circa 1965.
However, there is a perceptible slowdown in improvements from circulatory diseases and a shift to deterioration from unspecified causes in recent years.
The deceleration in improvements relating to circulatory diseases could be linked with behavioural risk factors, such as obesity, lack of exercise and eating habits. Equally, it’s possible that the potential for further improvements from circulatory diseases might simply be exhausted.
Clearly, neoplasms are casting a longer shadow on mortality, and the development of new cancer drugs and treatments will influence the potential for future mortality improvements. Unlike with cardiovascular diseases, every cancer site has different causes and factors that influence the disease and therefore requires its own therapy and medicine.
While mortality improvements have slowed down in certain age bands, at present our analysis does not show a general indication for negative mortality trends in Germany for the future.
Endnote
- Longevity risks and hence ages of 60 and older representing the main scope of annuity products were not the subject of our investigation.





