-
Property & Casualty
Property & Casualty Overview

Property & Casualty
We offer a full range of reinsurance products and the expertise of our talented reinsurance team.
Expertise
Publication
Production of Lithium-Ion Batteries
Publication
Time to Limit the Risk of Cyber War in Property (Re)insurance
Publication
Generative Artificial Intelligence in Insurance – Three Lessons for Transformation from Past Arrivals of General-Purpose Technologies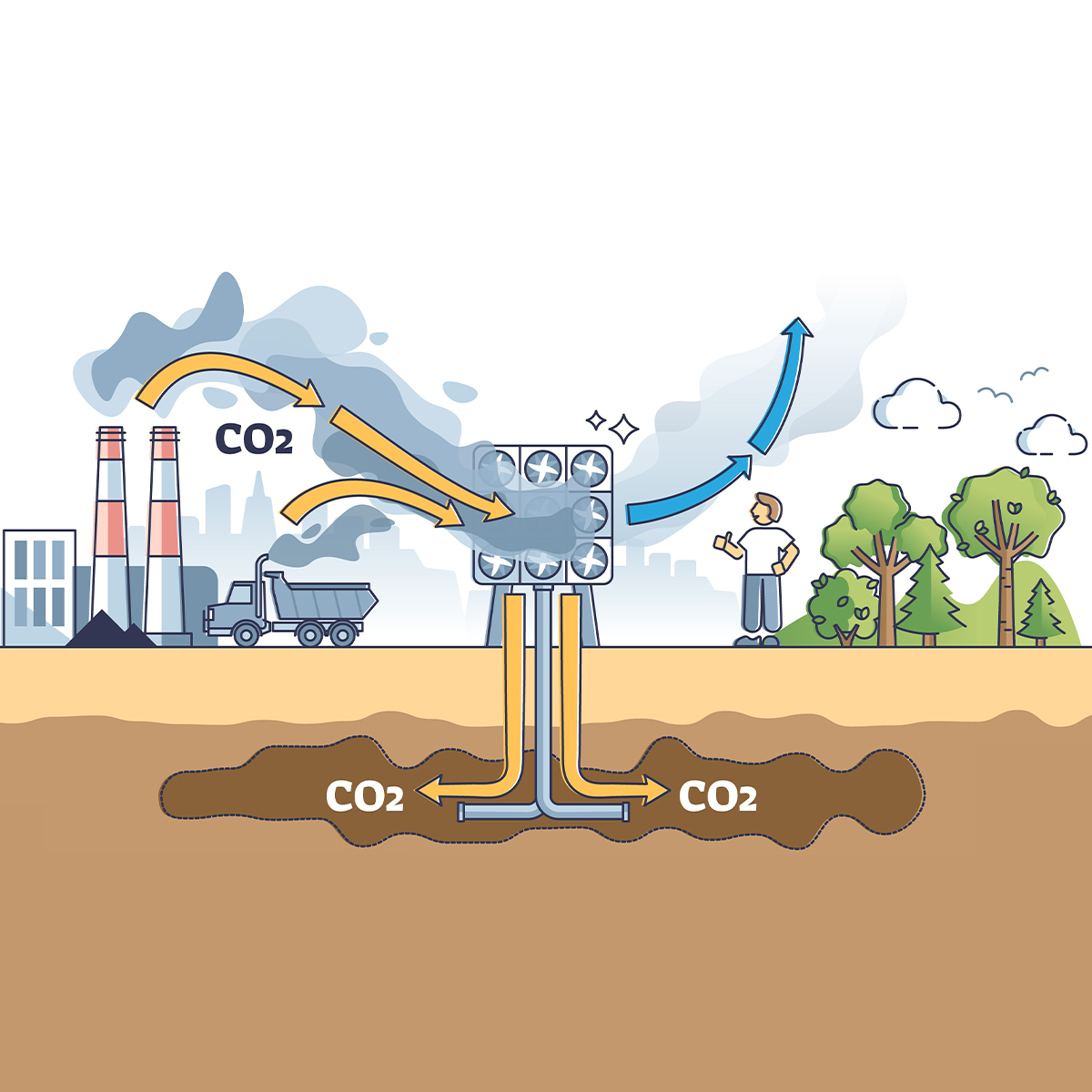
Publication
Human Activity Generates Carbon and Warms the Atmosphere. Is Human Ingenuity Part of the Solution?
Publication
Inflation – What’s Next for the Insurance Industry and the Policyholders it Serves? -
Life & Health
Life & Health Overview

Life & Health
Gen Re’s valuable insights and risk transfer solutions help clients improve their business results. With tailor-made reinsurance programs, clients can achieve their life & health risk management objectives.
UnderwritingTraining & Education
Publication
The Key Elements of Critical Illness Definitions for Mental Health Disorders
Publication
What Are We to Make of Cannabis Use in The Insured Population? Business School
Business School
Publication
Knife or Needle: Will the New Weight Loss Medication Replace Bariatric Surgery?
Publication
Weight Loss Medication of the Future – Will We Soon Live in a Society Without Obesity? Moving The Dial On Mental Health
Moving The Dial On Mental Health -
Knowledge Center
Knowledge Center Overview

Knowledge Center
Our global experts share their insights on insurance industry topics.
Trending Topics -
About Us
About Us OverviewCorporate Information

Meet Gen Re
Gen Re delivers reinsurance solutions to the Life & Health and Property & Casualty insurance industries.
- Careers Careers
How the Pandemic Could Shape the Future of the Group Risk Market in the UK

September 16, 2021
Joanne Kuller,
Michael George
Region: United Kingdom
English
In 2020 the UK’s Group insurance industry hit an all-time high in pay-outs, as claims amounting to just over GBP 2 billion were paid out to beneficiaries according to Group Risk Development (GRiD).1 This was almost 15% above what was paid out in 2019 and around GBP 100 million of these claims were Group Life claims related to COVID‑19. The Group Risk market has responded to this challenge by demonstrating its importance and resilience. The pandemic has given the industry an opportunity to review existing processes and highlight the true importance and value of the benefits it offers. Below we explore how the pandemic might shape the Group Risk market going forward.
Attitude to concentration risk
In the UK across Group Life policies, it is common practice to put in place event limits, which cap the exposure liability to a maximum amount if a catastrophic event – such as a terrorist act – were to occur. The likelihood of reaching an event limit increases with the number of people working in offices. When the pandemic first hit and workers made the shift to working from home, a reduction in the number of people occupying office space naturally ensued. As many workplace studies have already shown, this way of working is likely to continue post pandemic, which may result in a reduction in concentration risk going forward.
Permanent changes in working practices may lead to a change in approach when it comes to offering capacity and managing exposure risk. Insurers might take different views on occupancy rate assumptions (the average number of people expected to be working in an office) as well as event limits, if the number of employees within office buildings remains low (or at least lower than pre-COVID‑19 levels). Scheme sponsors may also take this as an opportunity to review their requirements in terms of event limit coverage.
Equally, if Group Life event limits are being reconsidered, there may also be a reassessment of event limits in the context of Group Income Protection cover. Is it time for the industry to consider the risk that catastrophic events pose to the Group Income Protection market? It wouldn’t seem unreasonable, given the scale of loss insurers may be exposed to, should such an event occur.
Additions to cover
Many Group policies offer additional services to employees – such as bereavement and probate helplines, financial assistance, mental health apps to assist employees in times of need – and online doctors, who can help with diagnosis or triaging. It is no surprise that the pandemic has resulted in higher stress and anxiety levels amongst the general population – from the financial stress of family members losing jobs to health concerns related to the pandemic and its short- and long-term impacts. The pandemic has helped highlight some of these services, compared to pre-pandemic times when employees may not have known they existed or understood their importance.
According to research carried out by GRiD, interactions with such services have doubled over the past year and there has been a significant increase in usage of online and telephone support services (45% and 42% increase, respectively).2 Companies, such as Thrive, are leading the way in mental well-being. The Thrive app, which is the only NHS approved app in this space, provides in‑depth tools and support to assess and treat common mental health problems. These types of applications will be needed well beyond the pandemic.
Since the pandemic began, 63% of employers have increased support for their staff in at least one area across mental, financial, physical and social well‑being.3 To see employers doing more in the area of well-being, which evidently is valued by employees, is very encouraging. In addition, the recent Government response to the “Health is Everyone’s Business” consultation recognised the important role employers play in providing the right support to employees to minimise the risk of ill-health-related job loss. The government also agreed insurance policies that include access to high-quality services can be a valuable source of support and assist in supporting return to work.
In the future, we might expect these add‑ons to play more of a part in group policies and become more valuable to employees as awareness is increased, and perhaps price will not be the only factor in deciding which coverage to select.
Innovation in the Group Risk market
The pandemic has accelerated innovation in many markets, not least in the healthcare industry where professionals have observed the benefits of digitalisation first-hand over the past 18 months.
The Group market may also see an acceleration with the increased awareness and focus on health and well-being. Offering health and protection benefits to prospective staff may be a way of retaining and recruiting employees and in turn drive further growth and innovation, and the development of better automation and data gathering techniques. With these should come more efficient quote processes and greater insight, from good quality data feeding into the pricing process.
An online platform could assist with data gathering, allowing the employee and the employer to access past information and make any necessary changes easily. Many companies are making use of employee flexible benefit platforms, which have been successful in engaging employees. Is there a link between such platforms and group data automation?
The introduction of an industry-wide, consistent, simplified template could be created to readily provide membership data, so quotes could be priced quickly and more efficiently. Currently the majority of quotation time is spent on querying, manipulating and cleaning member data, which can often be a laborious exercise. A template that aims to standardise data would be something from which the whole market would benefit. While we appreciate the task wouldn’t be an easy one, with today’s data analytic capabilities, it should be achievable over time.
Digitalisation will certainly have a part to play in any type of innovation that takes place in the market. The use of platforms – such as LiveSmart’s digital health assessments – are already in use and will be a helpful tool in keeping policyholders healthy, especially given the importance placed on health and well-being as a result of the pandemic.
Adapting to pandemic disruptions
Cancer care and early screening in the UK have inevitably been disrupted due to the constraints on NHS resources because of COVID‑19, with 3 in 10 patients experiencing disruptions to their NHS cancer treatments.4 NHS waiting lists are growing and according to NHS England data, as of May 2021, 5.3 million patients were waiting for routine hospital care and the backlog of people waiting upwards of 52 weeks to start treatment was almost 340,000.5
Lack of intervention and postponement of treatments could result in an increase in the expected number of Group claims, following the pandemic. Indeed, any late diagnosis of conditions may result in claims that might otherwise not have arisen had the conditions been diagnosed and treated earlier. The delays to screening and backlogs we now face may result in heavier claims experience, which in turn may have an impact on future pricing, at least in the short term, until waiting times have normalised.
For Group Income Protection polices, the delays to treatment may lead to policy termination rates being lower than expected, as some employees can only realistically get back to work once they have received some sort of treatment for their condition. However, this is to some extent likely to be offset by the working-from-home environment, whereby the absence of a commute may mean some employees can continue to work where they would otherwise be unable. Going forward, it will be important for insurers and their clients to work together to establish return-to-work strategies and offer increased well-being support for employees.
Summary
The effects of the pandemic may well bring about some change to the Group Risk market in the future. Whether it be shifts in attitude towards concentration risk because of changing work patterns, or the short- to medium-term impact on Group claims due to the treatment backlogs faced at hospitals, change is likely. The increased awareness and usage of add‑on services to Group benefits has certainly already been a positive outcome for both employers and employees, and will continue to play an important role in Group benefit offerings. With an increased focus on health and well-being, this could accelerate growth and innovation for the industry.
Overall, although the COVID‑19 pandemic has caused some disruption to the Group Risk market, the market has also proved its resilience and emphasized the importance of group benefits to employees at such a difficult time.
Endnotes
- https://grouprisk.org.uk/2021/05/17/employee-benefits-magazine-group-risk-industry-paid-record-claims-to-employees-in-2020.
- Ibid.
- https://grouprisk.org.uk/2021/02/15/hr-wire-six-in-10-employers-have-increased-wellbeing-support-to-staff.
- https://news.cancerresearchuk.org/2021/08/05/patients-less-likely-to-rate-cancer-care-as-very-good-during-pandemic/.
- https://www.england.nhs.uk/statistics/wp-content/uploads/sites/2/2021/07/May21-RTT-SPN-publication-69343.pdf.


Michael George
Pricing Actuary



